What is Endometrial Cancer?
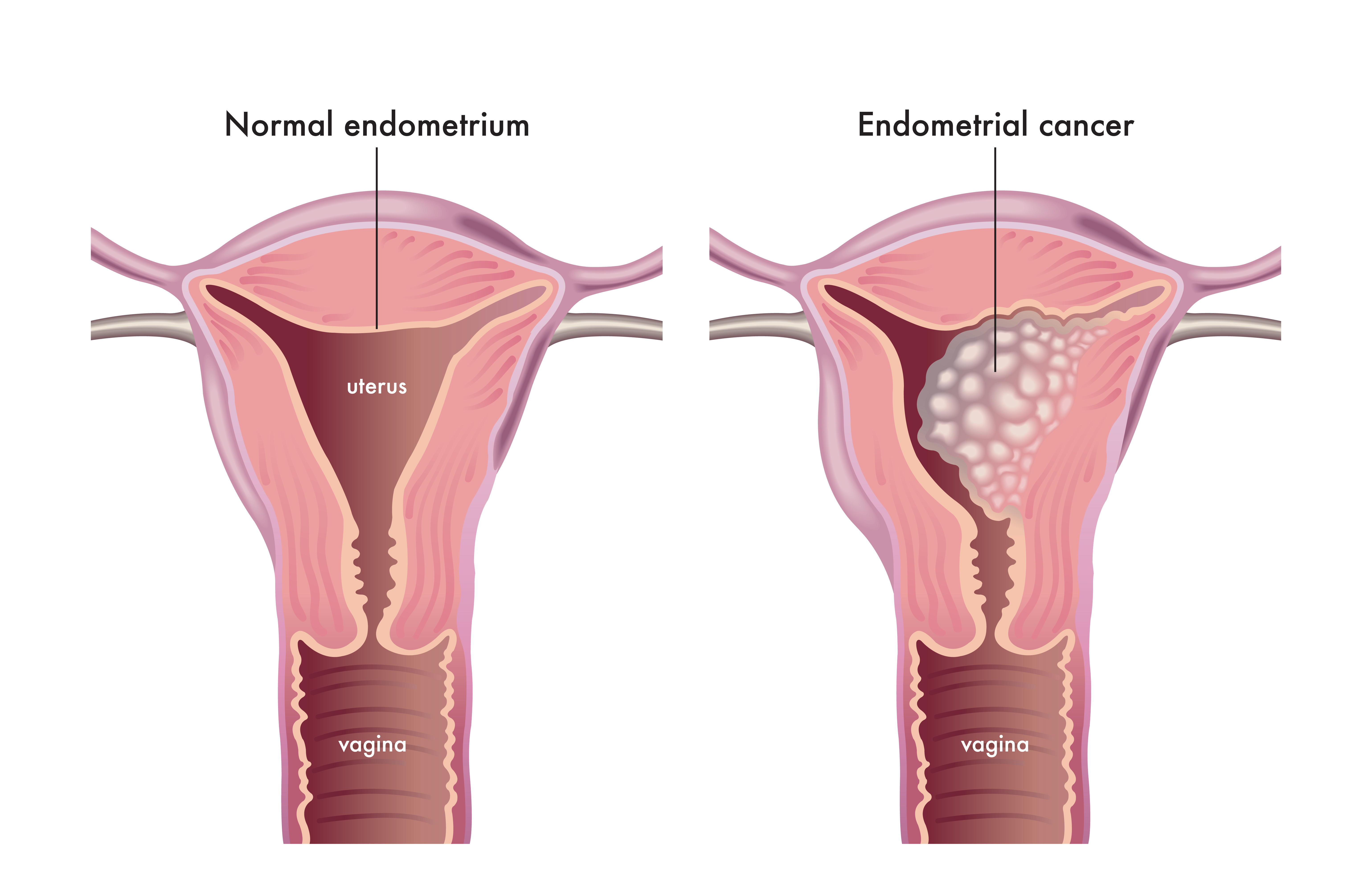
Endometrial cancer occurs when the cells that comprise the endometrium, the uterus’ inner lining, begin to rapidly grow out of control. The uterus is the female reproductive organ where a fetus grows during pregnancy. The upper portion of the uterus is called the body (or corpus, which means “body” in Latin). The cervix is located at the lower end of the uterus, joining the organ to the vagina. Endometrial cancer is the most common type of cancer found in the uterus.
The uterus’ body is comprised of two main layers, the myometrium and the endometrium. The myometrium is the thicker outer layer of muscle, which is used to push out a baby during childbirth. The endometrium is the thinner inner layer of the uterus. During the menstrual cycle, the endometrium changes due to changing levels of hormones. The hormone estrogen causes the endometrium to thicken in order to nourish an embryo if a pregnancy occurs. If no pregnancy occurs, lower amounts of estrogen are produced, and the hormone progesterone is produced instead. Progesterone causes endometrial lining to shed from the uterus, becoming the menstrual flow (period). This cycle will then continue until a woman reaches menopause.
Endometrial cancers are classified into different types, depending on what the cells look like under a microscope. The different classifications of endometrial cancers include:
- Adenocarcinoma, including less common types, such as clear-cell carcinoma, mucinous adenocarcinoma, undifferentiated carcinoma, dedifferentiated carcinoma, and serous adenocarcinoma.
- Uterine Carcinosarcoma
- Squamous Cell Carcinoma
- Small Cell Carcinoma
- Transitional Carcinoma
Endometrioid cancers are cancers that begin in gland cells and often look very similar to the normal uterine lining of the endometrium. Sub-variants of endometrioid cancers include:
- Adenocarcinoma
- Adenoacanthoma
- Adenosquamous
- Secretory Carcinoma
- Ciliated Carcinoma
- Villoglandular Adenocarcinoma
Uterine sarcomas are another form of cancer that can appear in the uterus. Uterine sarcomas begin in the myometrium, the muscle layer of the uterus, or uterus’ surrounding connective tissues. Common forms of uterine sarcomas include both uterine leiomyosarcomas and endometrial stromal sarcomas.
What causes endometrial cancer? What puts me at risk?
Scientists do not yet know what exactly causes endometrial cancer. However, we do know that mutations in the DNA of the cells that comprise the endometrium occur in order to lead to the development of endometrial cancers. DNA mutations force normal, healthy cells into abnormal, cancerous ones that multiply out of control. These cells then form a mass called a tumor. The cancerous cells can also invade nearby tissues, causing the tumor to spread elsewhere in the body (a process called metastasizing).
Genetic mutations have the potential to cause normal cells in the body to become cancerous. Inherited genetic mutations are a result of the genes we inherit from our family, especially immediate family like parents and grandparents. A portion of endometrial cancers occur in women that have inherited mutations that are linked to an increased risk of developing endometrial cancers. Genetic testing can detect such mutations.
The following factors have the potential to increase the chance of a woman developing endometrial cancers:
Hormonal Imbalances
Fluctuations in the two main female hormones produced in the ovaries, estrogen and progesterone, can cause changes in the endometrium. Diseases that may cause increases of one hormone and not the other can throw off your hormonal balance and increase your risk of developing endometrial cancer. Examples include diseases such as obesity, diabetes, polycystic ovarian syndrome (PCOS), or irregular menstrual/ovulation cycles. Additionally, taking hormone treatment for diseases such as breast cancer could also put you at an increased risk of developing endometrial cancer. If you are concerned about your risk of developing endometrial cancer due to any of these circumstances, consult your local primary care provider.
More Years of Menstruation
Women who begin menstruation at a young age, typically defined as twelve years and younger, and women who have delayed menopause are also put at an increased risk of developing endometrial cancers. The more menstrual cycles a woman’s body endures, the more exposure her endometrium has had to estrogen, increasing her risk to develop endometrial cancer at some point in her life.
Infertility or Never Having Children
Women who have never been pregnant are also at an increased risk of developing endometrial cancer than those who have.
Family History of Endometrial, Ovarian, and/or Colon Cancers
Women who have close personal or familiar histories with endometrial, ovarian, and/or colorectal cancers may have an increased risk of developing endometrial cancer. This is a result of many genetic linkages that exist amongst close family members.
Growing Older
Endometrial cancer is most common in women after they have hit menopause.
How do I know if I have endometrial cancer?
Endometrial cancer is commonly found in early stages as it typically results in abnormal vaginal bleeding. The following are common signs and symptoms of endometrial cancer:
- Unusual vaginal bleeding, spotting, or other discharge not relating to the menstrual cycle
- Postmenopausal bleeding
- Pelvic pain or a mass in your pelvis.
- Weight loss
- Pain or difficulty while urinating
- Pain during sex
Many of these symptoms can be caused by things other than cancer. If you are experiencing any of these symptoms, it is important to consult your primary care physician to have them checked out.
What is the best way to treat endometrial cancer?
Endometrial cancer is usually treated with surgery that removes the uterus, ovaries, and fallopian tubes. Other treatment options include radiation therapy, chemotherapy, hormone therapy, targeted therapies, and/or immunotherapy. Your oncologist will help you select the treatment option that best suits your endometrial cancer and your wishes as the patient. Here are some of the leading treatments for endometrial cancer, all of which are available at South Texas Oncology and Hematology for Cancer Care:
Surgical Options
Endometrial cancers are usually treated surgically with a hysterectomy, a procedure that removes the uterus, as well as the ovaries and fallopian tubes. Pursuing this surgical option aims to remove the cancer entirely and decrease your chances of it coming back. However, by having a hysterectomy, you will not be able to become pregnant in the future. Additionally, the removal of your ovaries will trigger menopause, if you haven’t already experienced it.
While performing your surgery, your oncologist will also observe the areas surrounding your uterus to ensure that the cancer has not spread. They may remove lymph nodes and surrounding tissues for testing in order to find out your stage of cancer.
Radiation
Radiation therapies use energy beams like X-Rays and protons to kill cancerous cells. Radiation therapies can be used before surgeries in order to shrink tumors and make them easier to remove. Additionally, radiation may be used to reduce your risk of cancer coming back after surgery.
Radiation can be received either from a machine outside of your body, or by being placed in your body. With external beam radiation, patients lie down while the machine directs the radiation to specific parts of your body to best treat your cancer. Internal radiation, also called brachytherapy, involves placing a small radiation-filled device in your body. For endometrial cancers, this typically looks like a small radiation-filled device such as small seeds, wires, or a cylinder being placed inside your vagina for a short period of time.
Chemotherapy
Chemotherapy drugs look for cells that divide quickly (like cancer cells) and destroy them. It is particularly useful when treating cancer in later stages because it can kill cancer cells throughout the whole body. More than half of cancer treatments involve some kind of chemotherapy, sometimes to completely remove the cancer and sometimes to just slow symptoms. You might have heard of chemotherapy side effects such as hair loss, nausea, or damage to the skin and/or bones. These side effects occur because the tissues in your hair, intestines, skin, and bones are all fast-growing cells and thus might potentially be attacked by chemotherapy drugs.
Chemotherapy drugs can be taken orally or injected into your veins. Your doctor may recommend chemotherapy before your surgery to shrink the cancer to more easily treat it or following your surgery to decrease the risk of your cancer returning. Chemotherapy may be useful in treating endometrial cancer that is advanced or recurrent, especially if it has spread beyond the uterus.
Hormone Therapy
The aim of hormone therapies is to lower the hormone levels in the body through taking specific medications. As a result, the cancer cells that require these hormones to continue growing die. Hormone therapy can be effective with endometrial cancers that are advanced or have spread beyond the uterus.
Targeted Drug Therapy
Targeted therapies are better at attacking only cancer cells while sparing healthy body cells. In some cases, targeted therapies do not cause as many side effects as other treatments as they are more effective at targeting only cancer cells. Your oncologist may recommend combining targeted drug therapies with chemotherapy to treat endometrial cancers that are advanced.
Immunotherapy
Immunotherapy drugs boost your immune system’s natural ability to fight your tumor. Tumors are good at avoiding the body’s immune system, so to improve your body’s response, immunotherapies include a variety of strategies such as adding extra T-cells and antibodies that specifically recognize and attack your tumor, introducing vaccines, or blocking the signals that would normally tell the immune system to slow down. In the case of endometrial cancers, immunotherapy may be an option if the cancer is advanced and has not responded positively to other forms of treatment.
How can i prevent endometrial cancer?
There is no guaranteed way to prevent developing endometrial cancer. However, some ways you can decrease your risk of developing endometrial cancers include:
Staying at a Healthy Weight
Women who experience obesity are almost three times as likely to develop endometrial cancer than women who are at a healthy weight. Staying within a healthy weight range is one way to lower your risk of developing endometrial cancer.
Staying Physically Active
Scientists have found linkages between higher levels of regular physical activity and lower risks of developing endometrial cancer. Active lifestyles and regular physical activity have many benefits that can help to lower your risks of developing endometrial cancer, including helping you achieve and stay at a healthy weight and lowering your risk of both high blood pressure and diabetes.
If You Receive Hormone Therapy – Discuss the Pros and Cons with your Doctor
Some women elect to use estrogen in order to treat their symptoms of menopause. This can occur in many different forms, including pills, shots, skin patches, creams, and/or vaginal rings. If you are considering about taking a form of estrogen to manage your symptoms of menopause, it’s advised to talk with your doctor about how they may affect your risk of developing endometrial cancer. Progestins, which are progesterone-like drugs, have the potential to reduce the heightened risk of developing endometrial cancer in women who partake in estrogen therapy; however, this combination has the potential to increase your risk of other cancers like breast cancer. If you are considering any kind of hormone therapy, it is highly recommended to discuss all your options and their potential side affects thoroughly with your doctor.
Treat Endometrial Problems
If you have a history of endometrial disorders or problems, getting the proper treatment can help decrease your risk of developing endometrial cancer. Many forms of endometrial cancers take years to develop, and many are known to originate from small, less serious changes in the endometrium. These changes are called endometrial hyperplasia, which may go away on its own, but often must be treated with hormones or surgery.
The most common sign of endometrial problems and cancers is abnormal vaginal bleeding. If you are experiencing this, make sure to see your healthcare provider as soon as possible to get it checked out.
Talk With Your Doctor if You Have HNPCC
Women who were diagnosed with hereditary nonpolyposis colon cancer, also called Lynch syndrome, have a high risk of developing endometrial cancer. Many oncologists will recommend that women with HNPCC have a hysterectomy and bilateral salpingo-oophorectomy in order to remove her uterus, ovaries, and fallopian tubes. In many cases, this procedure can wait until after a woman is finished having children, however, it is advised that you talk to your physician about what options are the safest for you.
References
https://www.cancer.org/cancer/types/endometrial-cancer/about/what-is-endometrial-cancer.html
https://www.mayoclinic.org/diseases-conditions/endometrial-cancer/symptoms-causes/syc-20352461
https://www.cancer.org/cancer/types/endometrial-cancer/detection-diagnosis-staging/signs-and-symptoms.html
https://www.mayoclinic.org/diseases-conditions/endometrial-cancer/diagnosis-treatment/drc-20352466#:~:text=Treatment%20for%20endometrial%20cancer%20is,that%20cancer%20cells%20rely%20on
https://www.mayoclinic.org/diseases-conditions/endometrial-cancer/diagnosis-treatment/drc-20352466#:~:text=Treatment%20for%20endometrial%20cancer%20is,that%20cancer%20cells%20rely%20on