- What is Prostate Cancer?
- Prostate Cancer Statistics
- Signs and Symptoms of Prostate Cancer
- Risk Factors and Causes of Prostate Cancer
- Prostate Cancer Prevention
- Screening and Early Detection of Prostate Cancer
- Tests to Diagnose Prostate Cancer
- Treatments for Prostate Cancer
- How to Prepare for your Appointment
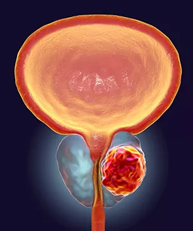
Prostate cancer begins in the prostate gland. The prostate gland is only found in males and is responsible for creating some of the fluid in semen.
Cells in the body grow uncontrollably when cancer starts to form. Most types of prostate cancers are known as adenocarcinomas, which develop from gland cells that create prostate fluid for semen.
Although rare, below are some other forms of prostate cancer that could develop:
- Sarcomas
- Small cell carcinomas
- Transitional cell carcinomas
- Neuroendocrine tumors
If you were diagnosed with prostate cancer, it’s likely an adenocarcinoma. Most types grow slowly, but some can multiply and quickly spread throughout the body. In many cases, men who die due to other factors never even knew they had prostate cancer. Sometimes the symptoms aren’t noticeable or don’t affect someone’s life significantly enough to seek medical care.
According to medical research, a pre-cancerous condition could develop into prostate cancer. However, this has not yet been proven. Conditions like this are often found during a prostate biopsy. During this procedure, a doctor removes a small piece of the prostate to determine if there are cancerous cells. When examined under a microscope, prostate gland cells could look like they’re changing, but without growing or spreading to other areas like abnormal cancer cells would.
These abnormal patterns fall under two prostatic intraepithelial neoplasia (PIN) classifications:
- Low-grade PIN - Prostate cell patterns almost look normal
- High-grade PIN - The cell patterns appear to be abnormal
A low-grade PIN doesn’t seem to affect a man’s risk of developing prostate cancer at some point in his life. However, researchers believe that a high-grade PIN could indicate a pre-cancerous condition. If your doctor takes a biopsy of your prostate and finds a high-grade PIN, there could be a chance that prostate cancer forms at some point in your life.
Just because you have a high-grade PIN does not necessarily mean you will develop prostate cancer. These findings are not absolute, so you should always consult with an experienced medical provider about your risk factors.
After skin cancer, prostate cancer is the most common cancer in American men. The American Cancer Society estimates that around 191,930 new cases will be diagnosed in 2020 in the United States. Of every nine men, about one will develop prostate cancer in their lifetime. It is the second-leading cause of cancer death, killing around one of every 41 men.
Around 60 percent of new cases develop in men over 65 years old. It’s rare for someone under the age of 40 to develop prostate cancer. The average age for receiving this diagnosis is 66 years old. Additionally, 90 percent of patients are diagnosed when it’s in the local or regional stage. That means it is only in the prostate and nearby organs and has not yet spread to other regions of the body.
Prostate cancer might not cause any symptoms, especially when it’s in the early stages. Some signs and symptoms are similar to other diseases and ailments, so you must speak with a doctor to determine your diagnosis.
Prostate cancer symptoms in advanced stages include:
- Blood in the semen or urine
- Pain in the back, chest, hips, or other parts of the body where it spread to the bones
- Difficulty urinating, including the urge to urinate more frequently or a weak or slow urinary stream
- Numbness or weakness in the feet or legs
- Loss of bowel or bladder control if the cancer is pressing against the spinal cord
If you notice any of the symptoms above, you should immediately make an appointment with a medical provider. Most of these symptoms can be the result of another ailment. For instance, non-cancerous growth of the prostate, known as benign prostatic hyperplasia (BPH), can cause trouble urinating. You might have a less serious condition that’s causing your symptoms; however, you should see a specialist so they can perform tests and screen for prostate cancer.
Researchers are unsure of the exact causes of prostate cancer. They have found possible risk factors and how they could lead to the development of cancerous cells. When cancer forms in the prostate, it’s because of changes to the cell’s DNA. DNA makes up a person’s genes and controls cells, deciding when they divide, grow, and die.
Oncogenes are responsible for helping cells divide, stay alive, and grow.
Tumor suppressor genes repair mistakes in a person’s DNA, control cell growth, and cause cells to die when they should.
DNA mutations could turn on oncogenes or turn off tumor suppressor genes and cause cancer to develop. When this happens, cells grow uncontrollably and divide to form new abnormal cells. These changes to someone’s DNA could be acquired throughout their life or inherited from one of their parents.
Inherited gene mutations are passed down from one generation to the next. These mutations can be found in every cell. Cancer associated with inherited genes is known as hereditary cancer.
Below are various mutated genes that have a possible link to hereditary prostate cancer:
- HOXB13 - Assists in prostate gland development. This type of mutation is rare but has been linked to early-onset prostate cancer.
- DNA mismatch repair genes (MSH6, MSH2, MLH1, and PMS2 - These genes fix DNA mistakes when a cell is getting ready to divide. Lynch syndrome (hereditary non-polyposis colorectal cancer) is a condition that occurs when there’s inherited mutations in any of these genes. It increases the risk of prostate, colorectal, and other forms of cancer.
- BRCA1 and BRCA2 - Tumor suppressor genes responsible for fixing DNA mistakes or causing a cell to die if it isn’t possible to fix the mistake. Mutations mostly cause ovarian and breast cancer in women but could also cause prostate cancer.
- RNASEL (formerly HPC1 - Tumor suppressor genes cause cells to die when there’s a problem inside them. Mutations allow abnormal cells to live.
- CHEK2, PALB2, ATM, and RAD51D - Genes that aid in repairing DNA
Acquired gene mutations occur when genes mutate throughout someone’s life instead of getting a mutation from a parent. Mutations associated with prostate cancer are more due to acquired gene mutations than inherited gene mutations.
The risk factors below could increase the chance of developing prostate cancer:
- Family History - Family history of breast cancer or genes that increase the risk, such as BRCA1 or BRCA 2. Also, having a blood relative who was diagnosed with prostate cancer could increase your risk.
- Age - It’s common for prostate cancer to form after 50 years old. As you get older, the risk increases.
- Race - Black people have an increased risk over other races. It’s also likely to be more advanced or aggressive.
There have been studies of other possible risk factors with inconsistent results, such as:
- Obesity - The risk of prostate cancer overall does not seem to be related to obesity. Some studies found that obese men have a lower risk of developing a slow-growing type of prostate cancer but a higher risk of advanced prostate cancer.
- Diet - There could be a slightly greater risk for men who eat a lot of dairy. Consumption of calcium through supplements or food could also increase the risk. However, most studies have not found an absolute link.
- Chemical exposure - Studies have shown there could be an increased risk for firefighters exposed to certain chemicals. Agent Orange, which was used during the Vietnam War, could have a possible link to prostate cancer, although there is limited evidence.
- Smoking - Some researchers found that smoking could slightly increase the risk. However, most studies haven’t found conclusive evidence.
- Vasectomy - There might be a small risk for prostate cancer in men who had a vasectomy.
- Prostate inflammation - Inflammation of the prostate gland is called prostatitis. Some studies show an increased risk of prostate cancer. Inflamed prostate tissue samples taken during a biopsy often contain cancer. However, researchers are still studying this possible link.
- Sexually transmitted infections - There isn’t a conclusion on whether STIs can lead to prostate cancer. Researchers believe there could be a link because certain sexually transmitted diseases, such as chlamydia and gonorrhea, cause inflammation.
There is ongoing research to determine the exact risk factors and causes of prostate cancer. If one or more of the factors above apply to you, there’s a chance you might not develop the disease. Nothing has been proven yet. If you’re worried about your risk of getting prostate cancer, you could consult with your doctor about making changes to your lifestyle.
There is no known way to prevent prostate cancer. There are conflicting studies and research that have not provided valid evidence for prevention. However, there are steps you could take that might lower the risk. Although you can’t change your family history, age, and race, there are changes to your lifestyle you could make.
Always talk to a medical professional before taking certain measures that could affect your overall health. If you possess specific risk factors for developing prostate cancer, your doctor might recommend changing your diet, exercising more, or taking vitamins.
Healthy Diet – Some studies found that consuming more vegetables and fruits or switching to a low-fat diet might reduce prostate cancer risk. You could try the following:
- Fruits and vegetables - Consider increasing the number of vegetables and fruits you eat every day. They are packed with nutrients and vitamins. Try adding another serving of fruits and veggies to your meals or eat them as morning or afternoon snacks.
- Low-fat-diet - Fatty foods, such as dairy products, meat, nuts, and oils, could increase prostate cancer risk when consumed in large amounts. Although there isn’t a proven link between fats and prostate cancer, there are various health benefits of reducing the number of fats you eat. Choose low-fat options, such as lean meat and low-fat yogurt to improve your heart health and control your weight.
- Dairy - Fatty foods, such as dairy products, meat, nuts, and oils, could increase prostate cancer risk when consumed in large amounts. Although there isn’t a proven link between fats and prostate cancer, there are various health benefits of reducing the number of fats you eat. Choose low-fat options, such as lean meat and low-fat yogurt to improve your heart health and control your weight.
Drugs - Multiple studies concluded certain medications could reduce a man’s risk of developing prostate cancer.
- Aspirin - Researchers still need to study aspirin's effects on prostate cancer risk. However, there’s some evidence that might support taking aspirin daily. You should discuss this with your doctor before you begin any type of regimen. Long-term use could cause medical issues, such as bleeding of the digestive tract.
- 5-Alpha Reductase Inhibitors - 5-alpha reductase is an enzyme that converts testosterone into dihydrotestosterone (DHT). DHT is a hormone that causes prostate growth. Inhibitors can prevent the enzyme from making DHT. Results from a study involving the drug and a placebo showed that the risk of developing low-grade prostate cancer was lower. However, there was a slightly increased risk of getting higher-grade cancer. High-grade prostate cancer could grow and spread. Your doctor could prescribe a 5-alpha reductase inhibitor, but it’s important to realize that the Food and Drug Administration has not approved it to prevent prostate cancer. There are also sexual side effects it could cause, such as erectile dysfunction and reduced sexual desire.
- Exercise - Since one of the potential risk factors of prostate cancer is obesity, you should increase your physical activity. Not only could exercising reduce your risk of developing prostate cancer, but it could also improve your health overall. It boosts mood and maintains weight. Exercise could also reduce your risk of heart disease and other forms of cancer. Doctors recommend a BMI between 18.5 and 24.9. Use the BMI calculator to check yours.
Prostate cancer could be found early if you undergo a screening. Screening is a way to test for signs of cancer before symptoms even develop. If the results show any abnormalities, you might need a biopsy to determine if you have cancer. Some medical organizations find these tests controversial, especially if they are performed on healthy individuals who haven’t shown symptoms of the disease. No one knows if the benefits outweigh any possible risks. You should discuss this with your doctor so they can review your medical history, risk factors, and other information to determine if you should undergo screenings.
The two main screening tests include:
- Prostate-specific antigen(PSA) blood test - PSA is a protein made in the prostate gland for semen. It can also be found in the blood. As your PSA level rises, the chance that you have prostate cancer also increases. There isn’t a specific level that indicates whether there’s cancer. Some doctors will decide additional testing is necessary if there’s a PSA of 2.5 or 3, while others will recommend it if the level is 4 or higher.
- Digital rectal exam - A doctor will lubricate a glove and insert one finger into the rectum to feel for hard areas or bumps on the prostate that could indicate cancer. A rectal exam is not as effective as a PSA test but might detect prostate cancer if someone has a normal PSA level.
If you undergo a screening and the results come back abnormal, your doctor might suggest other tests to determine whether you have prostate cancer. There are various tests you could undergo, but the only way to definitively diagnose prostate cancer is with a biopsy. The tests below are performed to check your risk factors and indicate if there’s abnormal cells or tumors.
The first thing a doctor will need to do is perform a physical exam and discuss your medical history. They will ask about specific symptoms you’ve been experiencing and how long they have been occurring. They will also ask if you have a family history of prostate cancer and your potential risk factors. They will check your body for unusual bumps, moles, and other abnormalities. They might also decide to do a digital rectal exam to feel for bumps on the prostate.
After the initial appointment, your doctor might refer you for imaging tests, such as:
- Magnetic resonance imaging(MRI) - This type of test uses strong magnets and radio waves to create images of the body’s soft tissue. A doctor can see the prostate and surrounding areas with an MRI scan.
- Computed tomography(CT)
- Bone scan - When prostate cancer metastasizes (spreads) to distant body parts, it typically reaches the bones. Determining if your form of cancer spread to the bone can be done with a bone scan. The doctor will inject a low-level radioactive substance and use a camera to detect radioactivity within damaged areas of your bones.
- Transrectal ultrasound (TRUS) - During this procedure, a doctor will insert a small probe into your rectum. This device gives off sound waves to create echoes, and a computer creates a black-and-white image. It can show abnormal areas of the prostate and measure the size of the prostate gland.
If any of the tests above indicate that you might have prostate cancer, a biopsy will likely be the next step. A doctor will remove small samples of the prostate and send it to a lab for examination under a microscope. It can take anywhere from one to three days or longer to get the results.
The report could include any one of the following results:
- Suspicious - There is an abnormality, but it isn’t necessarily cancerous
- Positive - The samples contain cancer cells
- Negative - The samples don't contain cancer cells
If cancer is present in your biopsy sample, a grade will be assigned to it. That indicates how aggressive it is. A doctor will examine your cancer cells and healthy cells to determine how they differ. A higher grade means the cancer is more aggressive and could spread throughout the body quickly.
Two types of techniques to assign a grade to prostate cancer are:
- Genomic testing - This analyzes the cancer cells and determines the type of gene mutations you have
- Gleason score - This score combines two numbers between 2 and 10 to indicate the level of aggressiveness; 2 is nonaggressive cancer, and 10 is a very aggressive cancer
After diagnosing you with prostate cancer, the doctor will need to determine if it spread to nearby lymph nodes, organs, or distant body parts. This is known as staging.
Each stage indicates the following:
- The extent of the primary tumor (where the tumor originated)
- If it spread to lymph nodes near the primary location
- If it metastasized (spread) to other areas of the body
- PSA level
- Grade group
Your doctor could recommend any of the following imaging tests if they believe cancer spread to other body parts:
- Ultrasound
- CT scan
- MRI
- Bone scan
- PET scan
Your treatment options will depend on the stage of your cancer, medical history, and other factors. If you have low-grade prostate cancer, you might not need to undergo immediate treatment. Some people don’t need treatment at all and just have to monitor their symptoms and attend regularly scheduled appointments to detect if the cancer is progressing. This is known as active surveillance and observation.
Surgery could be the right choice for you if the cancer is only located in the prostate gland. Two types of surgery include:
- Retropubic surgery - The surgeon makes one long incision in the abdomen to remove the prostate gland
- Robot-assisted laparoscopic prostatectomy - The surgeon inserts a mechanical device through several small incisions in the abdomen. The instruments attached to the device remove the prostate gland. This is the more common technique used for most types of prostate cancer.
Radiation involves killing cancer cells with high-energy rays or particles. Two main types include:
- External beam radiation - A machine used outside the body focuses beams of radiation on the prostate gland. It can cure the early stages of prostate cancer or manage symptoms. Typically, treatment is five days a week and could last for several weeks
- Brachytherapy (internal radiation) - Also called interstitial radiation therapy or seed implantation. Radioactive pellets (seeds) get inserted into the prostate tissue and deliver radiation doses over a specific period.
Hormone therapy reduces androgens to stop them from stimulating cancer cells in the prostate. Androgens are a type of male hormone made by the testicles and adrenal glands. Lowering the levels can shrink cells or slow the progression of cancer.
Chemotherapy involves taking a drug intravenously or orally to kill cancer cells. This type of treatment is usually necessary if it spread to areas other than the prostate and isn’t responsive to hormone therapy.
Immunotherapy uses a person’s immune system in fighting prostate cancer. Cancer cells can produce proteins that the immune system doesn’t recognize as threatening the body. Instead of being attacked and destroyed, the cells are free to grow and spread. Immunotherapy stimulates the immune system so it can differentiate between healthy cells and cancer cells.
Targeted therapy involves using drugs to identify cancer cells and attack them without damaging normal cells. It can be a good option if hormone therapy doesn’t work on advanced or recurrent prostate cancer.
Your doctor should review the treatment options available and advise which ones would be best for your situation. When deciding which option you want to pursue, consider the following factors:
- Age and expected lifespan
- Other medical conditions you have
- Your feelings about beginning treatment immediately
- Your doctor’s opinion about beginning treatment immediately
- Stage and grade of the cancer
- Likelihood of curing or managing your cancer
- Possible side effects
You don’t have to decide what to do at your appointment. Although you might not be able to wait that long, you should give yourself at least some time to consider all your options and make the choice that’s best for you. You might even be able to seek a second opinion.
Make an appointment with your family doctor if your symptoms aren’t concerning or causing problems in your daily life. They will refer you to a urologist (a doctor specializing in the urinary tract) if they suspect you might have prostate cancer.
Since this can be a scary and overwhelming experience, you must prepare in advance so you know what you should do before the appointment and don’t forget to ask specific questions:
- Write down all the questions you have for the doctor.
- Make a list of the medications you’re taking. That includes supplements and vitamins.
- Write all symptoms you’ve been experiencing, even if they seem irrelevant or unrelated to prostate cancer.
- When you schedule the appointment, ask if there’s anything you should do to prepare, such as fasting or avoiding certain activities.
- Include a detailed list of recent changes, such as stressors or major life changes like moving into a new home.
- Ask your family about their medical history. Make a note if anyone had prostate cancer.
- Find someone to go to the appointment with you. You should not be alone during this difficult time in your life.
Contact Us
At South Texas Oncology and Hematology for Cancer Care, we have more than 35 years of experience providing advanced treatment for prostate cancer patients. Our dedicated staff will assist you in choosing the best options and give you hope for the future. We know cancer is scary. You can depend on us to educate you on the process, provide compassionate support, and work hard to meet your expectations. To find out more about the services we offer, call us at (210) 593-5700 or fill out our online form.