What is Cervical Cancer
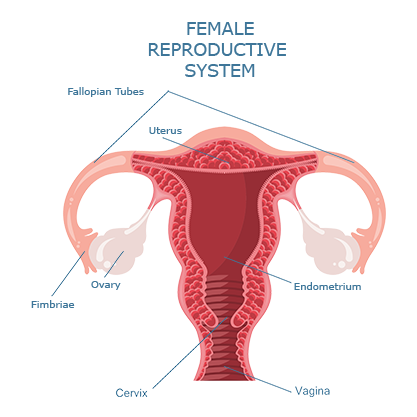
The cervix is a female reproductive organ that serves as a passageway for fluids to flow to and from the uterus. The cervix is the lowest part of a woman’s uterus, which is where a baby grows during a pregnancy. The cervix helps to connect the uterus to the vagina (which also serves as the birthing canal). During different phases of a woman’s menstrual cycle, the cervix can open and close to allow for the passage of fluids or to ease in pregnancy and childbirth. The cervix is comprised of two parts, each covered with a unique type of cells. The endocervix comprises the opening of the cervix, leading into the uterus. The endocervix is covered with glandular cells. The outer part of the cervix, which can be seen by a doctor during a speculum exam, is called the exocervix. The exocervix is covered in cells called squamous cells.
The place where glandular and squamous cells meet is called the cervix’s transformation zone. The transformation zone’s location changes as you age and if you become pregnant and give birth. The majority of cervical cancers originate in the cells of the transformation zone.
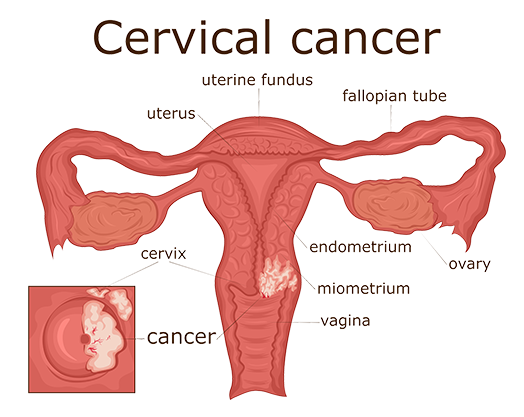
Cervical cancers originate on the surface of a woman’s cervix. Cells on the cervix may change to precancerous cells. These precancerous cells aren’t guaranteed to turn into cancer, but it is critical to find these potentially problematic cells and treat them in order to prevent cervical cancer.
The two main types of cervical cancers are called squamous cell carcinoma and adenocarcinoma. While more rare, cervical cancers can also appear as having features of both squamous cell carcinoma and adenocarcinoma.
Squamous Cell Carcinoma
Almost 90% of diagnosed cervical cancers present as squamous cell carcinomas. Squamous cell carcinomas develop from the cells present in the exocervix, and most often occur in the transformation zone at the joining of the exocervix and endocervix.
Adenocarcinomas
Adenocarcinomas develop from glandular cells, most often in the endocervix’s mucus-producing glands.
Mixed Carcinomas
Also called adenosquamous carcinomas, mixed carcinomas present features of both adenocarcinomas and squamous cell carcinomas. Most cervical cancers present as wither adenocarcinomas or squamous cell carcinomas. However, other types of cancer have the possibility to develop in the cervix. These types include melanoma, sarcoma, and lymphoma, all of which more often appear in other parts of the body. In the United States alone, about 14,000 people are diagnosed with cervical cancer annually. Diagnoses occur most frequently between the ages of 35 and 44. Death rates of those diagnosed with cervical cancer are on the decline, largely in part due to regular screenings for cervical cancer and the HPV vaccine.
What causes cervical cancer? What puts me at risk?
The majority of cervical cancers are caused by human papillomavirus (HPV). HPV is a commonly occurring sexually transmitted infection. There are many different types of HPV, some of which can lead to changes on a woman’s cervix that in turn cause cervical cancer to develop over time.
HPV is a very common sexually transmitted infection. While most people will get HPV at some point during their lives, many may not even realize it because their bodies will fight off the infection. If your body does not fight off HPV, however, it may cause the cells that cover your cervix to change to cancerous ones. The HPV vaccine has proven to be an effective protection against up to 90% of cervical cancer types. Additionally, regular screenings for cervical cancer with your primary health provider can help identify any cell changes before they develop into cervical cancers.
Other factors that put you at an increased risk of developing cervical cancers include being diagnosed with HIV (or any other diagnosis that would make it difficult for your body to fight viruses or other diseases) and smoking tobacco.
Signs of cervical cancer?
Regular gynecological screenings with a Pap smear can detect many types of cervical cancer. During a Pap smear, your gynecologist will collect cells from your cervix that are then examined for irregularities and signs of precancer. If your Pap smear comes back with irregularities, your gynecologist will recommend further testing. These tests could include HPV tests to check your cervix for HPV or the collection of tissue from your cervix to biopsy for cancer. If your biopsy suggests that you have cancer, your physician will order further testing to evaluate what stage your cervical cancer is at. These tests will likely include liver and kidney function studies, x-rays, and blood and urine tests.
Early cervical cancer often goes without symptoms and can be hard to detect outside of routine gynecological exams. Symptoms of cervical cancer in its early stages often include:
- Vaginal bleeding after menopause
- Vaginal bleeding and/or pelvic pain during or after sex
- Vaginal bleeding between menstrual periods, or menstrual periods that last longer or are heavier than normal
- Vaginal discharge that is more watery than normal, or that has an odor
Common symptoms of cervical that has advanced or spread beyond the cervix to other parts of the body include the previously noted symptoms of early-stage cervical cancer, in addition to:
- Difficult or painful urination or bowel movement
- The presence of blood in urine or bowel movements
- Dull backache Swelling in the legs
- Pain in the abdomen
- Abnormal fatigue
What is the best way to treat cervical cancer? Treatment for cervical cancer varies depending on the type and stage of cervical cancer you are diagnosed with. Additionally, treatment for cervical cancer can involve a combination of different treatments, rather than one. Here are some of the leading treatments for cervical cancer, all of which are available at South Texas Oncology and Hematology for Cancer Care:
Surgery
Surgery is a common treatment form for cervical cancer. The surgery you receive will be based on the type and progression of your cervical cancer. The following surgeries vary by invasiveness and should be discussed between you and your oncologist to determine the best course of treatment for you and your specific cancer.
Cold knife conization involves removing a cone-shaped portion of tissue from the cervical canal and the cervix. Depending on the circumstance, all or most of the cancer can be removed during this procedure if it is still in the early stages.
Sentinel lymph node biopsies remove the sentinel lymph node, which is the first lymph node that cervical cancers are likely to spread to once they spread from the primary tumor. If, from this biopsy, cancer is detected, your surgeon will remove this lymph node (as well as any other affected ones) and the rest of the cancer.
Hysterectomies are surgeries intended to remove the uterus. Depending on the progression of your cervical cancer, other surrounding structures may be removed in addition to the cervix. The following are common types of hysterectomies that may be used to treat cervical cancer.
- A total hysterectomy will remove both the uterus and the cervix. This procedure can be done through an incision on the abdomen (either laparoscopically or not) or completely through the vagina.
- A radical hysterectomy will remove the uterus and cervix, as well as portions of the vagina and ligaments and tissues that surround these organs. Depending on if the cancer has spread or not, the fallopian tubes, ovaries, and lymph nodes that surround these organs may also be removed.
- A modified radical hysterectomy will remove the same organs that a radical hysterectomy will, however, it removes fewer tissues surrounding the organs, helping to make the procedure less invasive.
Radical Trachelectomieswill remove the cervix, some upper portions of the vagina, and, depending on the circumstances, some surrounding tissues. Depending on the spread, surrounding lymph nodes may also be removed. With a radical trachelectomy, a woman’s ability to get pregnant is preserved. During this procedure, your surgeon will attach the uterus to the remaining portion of the vagina. Additionally, a stitch or band will be placed on the uterus to ensure the uterus can stay closed during pregnancy.
Bilateral salpingo-oophorectomies are typically done when the cervical cancer has spread to the ovaries and fallopian tubes. During this procedure, these organs are removed.
Radiation
In radiation therapies, high-energy x-rays are used to kill cancerous cells or prevent their growth. Radiation therapy can take one of two forms, either internal or external radiation therapy. External radiation therapies include the use of a machine to direct radiation towards the area of the body affected by cancer.
External radiation can occur through intensity-modulated radiation therapy (also called IMRT), which aims to prevent damages to nearby healthy tissues. With IMRT, a computer is used to make a three-dimensional rendering of the tumor’s size and shape. Once the tumor is mapped, thin beams of differing strengths are aimed at the tumor from a variety of angles.
Internal radiation therapies used radioactive substances that may be sealed within needles, seeds, catheters, or wires that are placed near or directly into the cancer.
Chemotherapy
Chemotherapy drugs look for cells that divide quickly (like cancer cells) and destroy them. It is particularly useful when treating cancer in later stages because it can kill cancer cells throughout the whole body. More than half of cancer treatments involve some kind of chemotherapy, sometimes to completely remove the cancer and sometimes to just slow symptoms. You might have heard of chemotherapy side effects such as hair loss, nausea, or damage to the skin and/or bones. These side effects occur because the tissues in your hair, intestines, skin, and bones are all fast-growing cells and thus might potentially be attacked by chemotherapy drugs. Chemotherapy drugs can be taken orally from injected into your veins.
Targeted Therapy
Targeted therapies are better at attacking only cancer cells while sparing healthy body cells. In some cases, targeted therapies do not cause as many side effects as other treatments as they are more effective at targeting only cancer cells. For cervical cancers, targeted therapy drugs will block the actions of specific enzymes and proteins that are involved in the spread and growth of cancerous cells. In treating cervical cancer, your doctor will test your cancer cells to determine the most effective targeted therapy for your cancer.
Immunotherapy
Immunotherapy drugs boost your immune system’s natural ability to fight your tumor. Tumors are good at avoiding the body’s immune system, so to improve your body’s response, immunotherapies include a variety of strategies such as adding extra T-cells and antibodies that specifically recognize and attack your tumor, introducing vaccines, or blocking the signals that would normally tell the immune system to slow down.
How can I prevent cervical cancer?
The two best ways to lower your risk of developing cervical cancer include getting your routine gynecological check-ups (most commonly through a Pap smear) and getting the HPV vaccine. Cervical cancers typically begin when cells change from being healthy to pre-cancerous. The most effective way to prevent cervical cancers is to prevent pre-cancerous cells from occurring at all, and to find and treat these pre-cancerous cells before they become invasive cancerous cells.
Depending on factors such as your age, personal risk for cervical cancer, and your overall health, you can take the following steps to prevent the development of pre-cancerous cells:
- Getting an HPV vaccine. HPV vaccines immunize children and young adults against certain HPV strains, especially those that are most commonly linked to cancer. While these vaccines can work to prevent an HPV infection, they do not treat against infections that are already there. The American Cancer Society typically recommends the HPV vaccination for children who are between the ages of 9 and 12. They do not recommend the vaccine for anyone over the age of 26. If you are concerned about the HPV vaccine, it is recommended that you discuss this option with your primary healthcare provider.
- Limiting your exposure to HPV. HPV can be passed from one person to another during any form of skin-to-skin contact with an HPV-infected part of the body. As HPV can be spread through any form of skin-to-skin contact, it is possible to be spread in ways other than sexual intercourse (while this is still one of the most common ways for it to be spread). HPV is a very common sexually transmitted infection, and it can be difficult to not be exposed to HPV at some time of your life. HPV can often go symptomless, so a person could have and pass on the virus to another without knowing.
- Using a condom during sexual intercourse. Condoms provide some protection against HPV, but because they do not cover every area of the body possible to become infected with HPV, they do not protect against it completely. Additionally, condoms help to protect against other sexually transmitted infections and HIV.
The following methods are options to find pre-cancerous cells in order to treat them before they become cancerous and invasive.
Pap smears are procedures performed by your gynecologist to collect cervical cells that can be examined to detect if there are any pre-cancerous or cancerous cells present. Pap smears can be done during your annual pelvic exams.
HPV tests are intended to detect forms of HPV that are most likely to cause pre-cancerous cells or cancer. The results of your HPV test will help determine your risk of developing cervical cancer. A positive HPV test will entail follow-up visits and testing, as well as the potential for a procedure to treat any found pre-cancerous cells. For any testing to detect pre-cancerous cells or cervical cancer, it is best to consult your primary care physician to see what tests or screening precautions you should consider.
References
American Cancer Society - What is Cervical Cancer
American Cancer Society / Can Cervical Cancer Be Prevented
CDC - What are the Risk Factors for Cervical Cancer
National Cancer Institute / Cervical Cancer Symptoms
National Cancer Institute / Cervical Cancer Treatment
The Cleveland Clinic / Health Library / Body Systems & Organs / Cervix