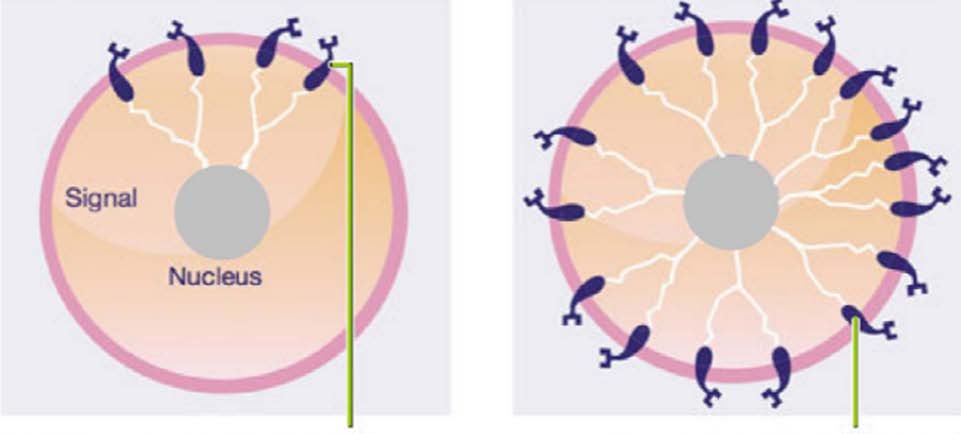
Triple Positive Breast Cancer (TPBC) is a type of breast cancer that occurs when the tumor cells grow due to estrogen (ER) and progesterone (PR) hormones, and a growth-promoting protein called human epidermal growth factor receptor 2 (HER2) on the cell surface.
When estrogen and progesterone attach to receptors (proteins) on the cell surface, they help “feed” the cells, making them grow out of control and spread.
Under normal circumstances, HER2 helps breast cells grow, divide, and repair themselves in an orderly manner. However, when something goes wrong with the gene that controls this HER2 protein, too many of these receptors can be made resulting in a rapidly growing and more aggressive type of breast cancer.
It is uncertain what causes breast cancer, but many studies point to a combination of factors, such as age, genetic predisposition, family history, reproductive factors, lifestyle behaviors and environment.
Breast cancer accounts for about 30% of all cancers diagnosed in the United States and this number has been increasing over the years. The National Cancer Institute predicts that in 2021, over 281, 500 women and 2,650 men will be diagnosed with breast cancer.
There are two main reasons that this number is increasing:
-
People have longer life expectancies vs. decades ago
-
People’s risk of getting breast cancer increases with age
- The median age at the time of diagnosis is 62 years old
-
People’s risk of getting breast cancer increases with age
-
Cancer screening and technology have dramatically improved over the years
- Clinical breast exams
- Risk tools that help predict a woman’s risk of getting breast cancer
- Screening tools such as mammograms and ultrasounds have highly improved technology, so breast cancers are being found at an earlier stage when it is most treatable and curable
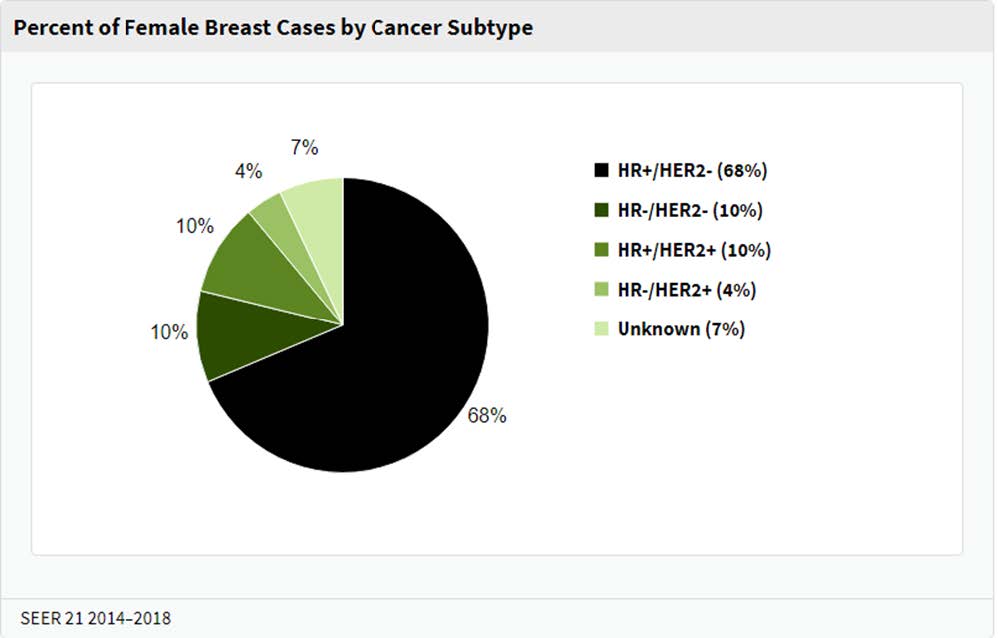
According to the National Cancer Institute, about 10% of breast cancer cases diagnosed in the United States are “triple negative breast cancers.”
A biopsy is the only definitive way to rule out or confirm a breast cancer diagnosis.
The specimen(s) removed during the biopsy is sent to a special lab where a pathologist, a doctor that studies diseases, examines the surgical specimen under a microscope to make a diagnosis.
When the pathologist finds that your cancer cells do not have estrogen and progesterone receptors, you are considered estrogen and progesterone negative. All patients diagnosed with an invasive breast cancer will have a special test, called an ImmunoHistoChemistry (IHC), to test for HER2.
The test will give a score of 0, 1+, 2+ or 3+:
-
IHC 0 or 1+ - the cancer is HER2-negative.
- HER2-negative cancers do not respond to drugs that target HER2.
-
IHC 2+ - the HER2 status of the tumor is not clear and is called "equivocal." Therefore, additional testing with FISH or DISH must be done to clarify the result.
- FISH - a special test that uses fluorescent pieces of DNA that will stick to the HER2 gene and can be counted under a microscope.
- DISH – a special test that uses stains to color HER2 genes so they can be counted under a microscope.
- The results of the FISH or DISH will be help determine a HER2-negative or HER2-positive diagnosis.
-
IHC 3+ - the cancer is HER2-positive.
- HER2-positive breast cancers are usually treated with drugs that target HER2.
Breast Imaging
Breast imaging tests such as a mammogram, ultrasound, and breast MRI take pictures of the inner part of your breast(s) so that a radiologist, a doctor that specializes in reading images, can take a closer look at your body.
-
Mammography uses X-rays to create images of your breasts
-
Screening Mammograms are done when there are no symptoms
- Example: annual mammograms
- Diagnostic mammograms are done when there is an area of concern
- 3D digital imaging or breast tomosynthesis is an advanced form of imaging that offers high-quality images from various angles, resulting in more accurate results vs. 2D imaging
-
Screening Mammograms are done when there are no symptoms
-
Ultrasound uses sound waves to create images of the breast tissue
- This procedure is often used in combination with a mammogram to evaluate areas of concern
- The procedure is painless
-
Breast MRI provides the clearest and most detailed pictures of the breast
- The MRI creates a 3-D image of the breasts
- Helps with staging and pre-surgery planning
- The procedure uses an IV contrast which is injected intravenously into the arm before the test. This contrast lights up during the exam, giving the doctor a better look at the breasts and surrounding areas
- The American Cancer Society recommends that all women that have a >20% lifetime risk of breast cancer, have a breast MRI and mammogram every year
Breast Biopsy
When a suspicious mass or an area of concern is seen on a mammogram or ultrasound, your doctor will order a breast biopsy to have a sample of the tissue examined to check for the presence of cancer cells.
After the tissue from the breast biopsy is removed, it is sent to a lab where a pathologist, a doctor that specializes in analyzing body tissue, examines the cells under a microscope and determines a diagnosis. The pathologist will interpret the tissue samples and prepare a report to share with the healthcare team.
The pathology report will contain some of the following information about the diagnosis:
- Procedure performed (type of biopsy)
- Specimen location (breast, axilla, lymph node(s), etc.)
-
Histology type (where the cancer originated in the breast)
- Ductal
- Lobular
- Phyllodes
- Other - such as tubular or mucinous
-
Grade status:
- Low - Grade I – cells look most like normal breast cells and are usually slow growing
- Intermediate - Grade II – cells look less like normal breast cells and are faster growing
- High - Grade III – cells look the least like normal breast cells and are usually fast-growing
-
Receptors/biomarkers status:
-
Hormone receptors
-
About 70-80% of breast cancers are hormone sensitive and include:
- Estrogen receptors (ER) and/or
- Progesterone receptors (PR).
-
About 70-80% of breast cancers are hormone sensitive and include:
- Hormone receptor positive breast cancers respond to hormone or endocrine therapy
-
Hormone receptors
-
HER-2 status:
- About 10% of newly diagnosed breast cancer patients are HER-2+
- HER-2+ is an over-expression of a protein called human epidermal growth factor receptor 2
- HER-2+ breast cancers respond to targeted therapies
-
Proliferation rate:
- Ki-67 – a test that measures the percentage (from 0-100%) of cancer cells that are actively dividing. The higher the proliferation rate, the faster the cells are growing and dividing
Your physician will stage your disease based on their findings. Staging determines the extent to which the cancer has developed and spread in your body.
-
Stage I (early stage)
- The cancer is small and has not spread to other areas of the body
-
Stage II and III
- The cancer is larger and has spread to nearby tissue and/or lymph node(s)
-
Stage IV (metastatic cancer)
- The cancer has spread to other areas of the body
Staging breast cancer helps the physician(s) plan treatments and predict your prognosis.
After a breast cancer diagnosis is confirmed, you will meet with a team of physicians that specialize in diagnosing and treating cancer to discuss your treatment options.
The treatment options include local treatment (surgery or radiation) or systemic treatment (medications given by intravenous catheter (IV) or by mouth).The type and order of treatment will vary based on your unique situation and can include a combination of the following:
- Surgery
- Radiation Therapy
- Chemotherapy
- Immunotherapy
- Hormone Therapy
- Clinical trials (for metastatic breast cancer patients)
Your team of physicians will work together to determine the best combination of treatments for you. They will take into consideration factors such as your age, overall health status, type of breast cancer and the stage of your disease.
Surgery
Surgery is a common treatment that is offered for early stage and locally advanced breast cancer. (Surgery is typically not done for stage IV breast cancers). When speaking with your surgeon, you will learn about the different surgical options that are recommended for you.
These recommendations will be based on many factors:
- Stage, tumor size and the location of your tumor
- Lymph node involvement
- The size of your breasts
- Your risk of cancer recurrence
- Age
- Personal preferences
Two of the main types of breast cancer surgeries are called partial mastectomy (also called lumpectomy) and mastectomy, which are performed by a surgeon. If you choose to have a mastectomy, you will have the option to have reconstruction surgery, which is performed by a plastic surgeon.
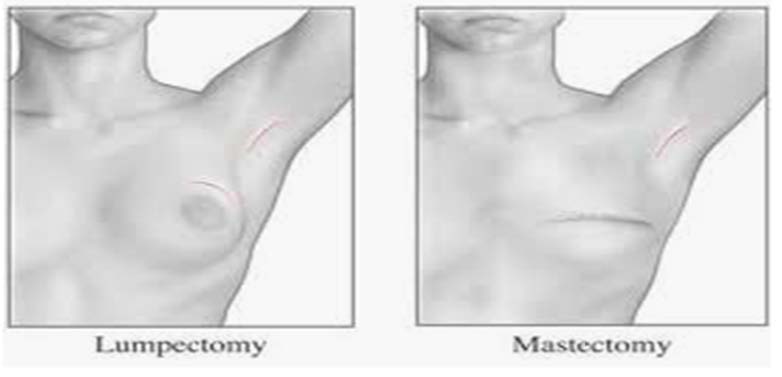
Partial Mastectomy or Lumpectomy
A partial mastectomy, also called lumpectomy, segmental mastectomy or quadrantectomy, is considered breast-conserving surgery (BCS). During surgery, the surgeon removes the tumor and a margin of surrounding healthy breast tissue. The goal of a partial mastectomy is to remove the tumor with negative margins, determine if the tumor has spread to lymph nodes, and to preserve the appearance and shape of the breast.
Axillary staging, a biopsy of underarm lymph nodes, is most often done in patients using a technique called sentinel lymph node mapping. (See “Types of Axillary Surgery”).
Mastectomy
A mastectomy is a surgical procedure involving the complete removal of the breast. Axillary staging, a biopsy of underarm lymph nodes, is done in most patients often using a technique called sentinel lymph node mapping. The goal of a mastectomy is the complete removal of the breast, removal of the underlying tumor with negative margins, and to determine if the tumor has spread to lymph nodes.
Following a mastectomy, a small amount of breast tissue will remain within the fatty tissue below the skin. The amount of breast tissue left behind is influenced by the type of mastectomy performed.
Mastectomies can be categorized into several different types:
- Nipple-sparing mastectomy – the breast tissue is removed preserving the overlying skin, nipple, and areola. This technique is utilized in patients pursuing breast reconstruction. Candidacy for nipple preservation is influenced by tumor factors and patient factors.
- Skin-sparing mastectomy – the breast is removed preserving the overlying skin but removing the nipple and areola. This technique is utilized in patients pursuing breast reconstruction.
- Total mastectomy - the breast is removed along with overlying breast skin, nipple, and areola. A total mastectomy leaves a flat contour to the chest following surgery.

Most insurance companies will cover the cost of mastectomy bras, breast forms, camisoles and prosthesis. Ask your surgeon to write a prescription for these medically necessary supplies.
Breast Reconstruction Surgery
Breast reconstruction surgery is a treatment option for you to consider if you choose a mastectomy. This procedure is done by a plastic surgeon, a physician who specializes in reconstructing the breast mound after a mastectomy.
The goal of breast reconstruction surgery is to restore your breast(s) appearance and help you feel better about your body and the way you look in clothing after having a mastectomy. The plastic surgeon will talk to you about your treatment options, all the while, keeping in mind your lifestyle and personal preferences.
The two main types of reconstructive surgery are breast implants and autologous reconstruction (using your own tissue to rebuild the breast mound). Keep in mind that every woman’s circumstance is different and recovery times post-surgery can vary greatly based on the type of surgery you choose.
Keep in mind that every woman’s circumstance is different and recovery times post-surgery can vary greatly based on the type of surgery you choose.
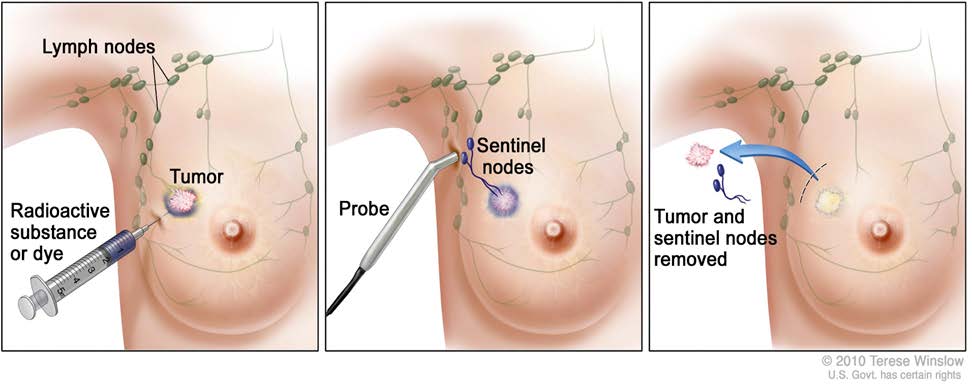
Types of Axillary Surgery
The axillary lymph nodes, lymph nodes located in the underarm area, are among the first places that invasive breast cancer spreads. Your surgeon will recommend a sentinel lymph node biopsy during surgery.
Sentinel lymph node mapping - radioactive dye is injected into the skin of the breast prior to surgery (can be done the day before surgery or several hours before surgery)
- This dye travels via the lymphatic vessels to the first lymph node(s)draining the breast, referred to as the sentinel lymph node(s).
- A radioactive probe identifies the lymph node(s) during surgery and is removed for analysis.
The goal of sentinel lymph node mapping is to accurately stage the axilla while limiting the extent of axillary surgery, thereby minimizing the risk of lymphedema (swelling of the arm area).
*Talk to your surgeon to learn more about lymph node removal during surgery.
Does Surgery Choice Affect Recurrence Rates?
A common dilemma that women face after a breast cancer diagnosis is deciding on the type of surgery to have in order to give them the best chance that the cancer will not recur.
Regardless of your surgery choice, long-term survival rates are the same, and local recurrence rates remain about the same when the standard of care is followed and are influenced by the following tumor characteristics such as the grade, size of the tumor and margin status.
In general, the risk of recurrence with the breast is as follows:
Partial Mastectomy or Lumpectomy
- Women who have a partial mastectomy followed by radiation therapy have about a 15% recurrence rate
- Women who have a partial mastectomy with no other treatment have about a 25 to 30% recurrence rate
Mastectomy
- Women who have a mastectomy will have a slightly lower risk in breast cancer recurrence compared to women who have a partial mastectomy with radiation
- Survival rates for women that have a mastectomy are the same as women who have a partial mastectomy with radiation
Nationally, the most common type of treatment for women with DCIS is a partial mastectomy followed by radiation therapy and endocrine therapy if the tumor is estrogen receptor positive.
Your healthcare team can help create a plan that is specific for you based on your medical history, tumor characteristics, and personal feelings.
Radiation Therapy
Radiation therapy is a local cancer treatment that uses high energy x-rays to kill cancer cells and shrink tumors. If you are a candidate for this type of treatment, you will be referred to a radiation oncologist, a physician who treats cancer with radiation therapy.
The radiation oncologist will likely recommend treatment based on several factors:
- After a partial mastectomy
- Helps lower the risk of the cancer coming back in the treated breast or in nearby lymph nodes
- After a mastectomy
- If the tumor is larger than 5 cm (roughly 2 inches)
- If cancer is found in the lymph nodes
- If the tumor involved the underlying muscle or skin
- If cancer has spread to other parts of the body
Radiation therapy is an outpatient procedure that typically starts after your surgical wound has healed (roughly 4 weeks). The radiation oncologist will set up a treatment plan specially designed for you through careful planning and mapping.
During this planning stage, you will be given special skin markings, which will aid in proper positioning for daily treatments. Radiation is given daily, Monday through Friday, for 3-6 weeks and each treatment takes only 10-15 minutes.
Side Effects of Radiation Therapy
Radiation therapy can have short-term side effects from treatment which typically resolve within two weeks of completing treatment:
- Swelling to the breast
- Skin changes to the treated area
- Sunburn appearance
- Redness
- Dry or flaky skin
- Darkening of the skin area being treated
- Fatique
- Pain to the treated area
- Hair loss to the treated area
- Sore throat (if treated to the supraclavicular lymph nodes)
Radiation therapy can have long-term side effects from treatment:
- Breast and skin changes such as discoloration, firmness, or shrinkage of the breast
- Lymphedema – if lymph nodes under the arm are treated, fluid may collect in the arm causing it to swell
Radiation therapy can have rare side effects from treatment:
- Rib fracture – with new protocols in place, this event is very rare.
- Lung problems – this event is a very rare occurrence but in some cases inflammation in the lungs can occur.
- Heart problems – with new protocols in place, this event is very rare.
- Increase the risk of a second cancer – this is a very rare occurrence.
If you have any questions or concerns or experience any of these side effects, talk to your radiation oncologist or nurse. They can explain more about your risk factors during treatment and recommended treatments to manage the symptoms.
The radiation oncologist will likely recommend treatment based on several factors:
-
After a lumpectomy
- Helps lower the risk of the cancer coming back in the treated breast or in nearby lymph nodes
-
After a mastectomy
- If the tumor is larger than 5 cm (roughly 2 inches)
- If cancer is found in the lymph nodes
- If the tumor involved the underlying muscle or skin
- If cancer has spread to other parts of the body
Radiation therapy is an outpatient procedure that typically starts after your surgical wound has healed (roughly 4 weeks). The radiation oncologist will set up a treatment plan specially designed for you through careful planning and mapping.
During this planning stage, you will be given special skin markings, which will aid in proper positioning for daily treatments. Radiation is given daily, Monday through Friday, for 3-6 weeks and each treatment takes only 10-15 minutes.
Medical Oncology
After receiving a breast cancer diagnosis, you can expect to see a medical oncologist at some point in your treatment plan. The medical oncologist has extensive knowledge in diagnosing and treating cancer and pays special attention to the pathology report(s) from your breast biopsy(s) and surgical pathology.
The information in the pathology report(s) helps the physician determine the best treatment option for the patient. In addition, the medical oncologist will discuss the risk of your cancer coming back after you have completed treatment.
Sometimes, additional testing (such as imaging, tissue sampling or genetic testing) will be needed to gather more information about your disease before a treatment plan can be established.
Once your treatment plan is established, the medical oncologist will recommend the medication(s) most beneficial to you. The medication is considered “systemic treatment,” because it affects the entire body, not just the breast.
The goal of systemic treatment is to kill cancer cells and reduce the risk of cancer coming back in the breast and in other parts of the body, such as the organs and bones.

Chemotherapy
Chemotherapy is an anti-cancer medication that is either infused intravenously or given orally (by mouth) to fight cancer. The medication affects you systemically, traveling throughout the body to kill cancer cells.
Chemotherapy is not indicated for all breast cancer patients, especially those with an early stage disease with favorable prognostics.
Your physician will weigh many factors to determine if you will need chemotherapy or not:
- Stage of the disease
- Prognostic status (estrogen/progesterone/HER-2)
- Size and location of the tumor
- Patient general health status
If your medical oncologist feels you are a candidate for chemotherapy, the timing of the treatment can vary based on many factors:
-
Neoadjuvant chemotherapy (NAC) - NAC is treatment (between 3 and 6 months) that is given before surgery with the goal of shrinking the tumor(s) or “downstaging tumors” before being removed with surgery.
- Most patients with larger tumors and/or positive lymph nodes benefit from NAC.
- Patients that are HER2+ will get targeted therapy along with the chemotherapy before surgery. After chemotherapy and surgery is completed, patients will continue with targeted therapy for a total of one year or in cases of metastatic disease, longer.
-
Adjuvant chemotherapy - Some patients with smaller tumors will be able to proceed to surgery first. After patients have healed from surgery, they will receive adjuvant therapy (treatment post-surgery).
- Patients that are HER2+ will get a combination of chemotherapy and targeted therapy during the initial treatment. Once chemotherapy is completed, the patient continues the targeted therapy for a total of one year or in cases of metastatic disease, longer.
- Adjuvant treatment kills any “floater” cells that may remain in the body after surgery and could potentially spread in the future.
Side Effects of Chemotherapy
There are a variety of different chemotherapy drugs available today for breast cancer treatment. Each drug has its individual list of possible side effects and they can be short-term or long-term, depending on the type and dosage of the drug(s) you receive.
The goal of chemotherapy is to kill the fast-growing and fast-dividing cancer cells. Since our body has many fast-growing healthy cells, chemotherapy will affect the cancer cells as well as some of the healthy cells (such as hair, skin, and the GI tract).
Fortunately, this effect is at a much lower rate and your body replenishes the cells quickly. The side-effects typically stop after you are done with treatment.
With the great advances in drug research, physicians understand the effects chemotherapy can have and will prescribe medications that will help lessen the expected symptoms.
We recommend that you to take the medications as prescribed and speak to your physician or nurse if you have any questions or concerns.
Some general side-effects of chemotherapy are as follows:
-
Short-term side-effects of chemotherapy:
- Hair loss
- Skin and nail changes
- Loss of appetite
- GI upset (nausea, vomiting, diarrhea, constipation, GERD)
- Fatique
- Low blood counts
- Bruising easily
- Higher risk of infection
- Mouth sores
- Nerve damage (neuropathy)
- Concentration problems (brain fog)
- Changes in menstrual cycle for younger women
-
Long-term side-effects of chemotherapy:
- Infertility
- Heart damage(rare)
- Bone thinning (osteopenia or osteoporosis)
- Leukemia (rare)
*Not all side effects are listed above. For more information on the possible side effects of chemotherapy, visit
www.chemocare.com.
Hormone Blocker or Endocrine Therapy
A hormone blocker or endocrine therapy is prescribed for hormone receptor positive tumors and is a type of “systemic treatment,” meaning it affects the entire body, not just the breast.
The goal of a hormone blocker is to kill cancer cells and reduce the risk of recurrence:
- Cancer cells have receptors (proteins) which attach to estrogen and progesterone and the hormones “feed” the cells, making them grow out of control and spread
- Hormone-blockers can either stop the hormones from attaching to the receptors or stop estrogen production
The medication comes in pill form and is taken daily for five years. However, some patients may benefit from taking the medication for 10 years or more, depending on the circumstances. A medical oncologist will help determine which medication is best for you based on your medical history, stage of disease and menopausal status.
Hormone-blockers are typically prescribed after local treatment (surgery or radiation therapy) has been completed. In some circumstances, a physician may prescribe the medication sooner if surgery is delayed or the disease has spread to other organs (not likely with DCIS). Patients who undergo a bilateral mastectomy may be able to avoid endocrine therapy post-surgery. Talk to your medical oncologist to see what option is best for you.
If your pathology report indicates that your cancer is hormone receptor positive, your medical oncologist will determine which medication is most beneficial to you based on your medical history and menopausal status.
Two types of hormone-blockers are:
- Tamoxifen - oral medication that blocks estrogen from attaching to cancer cells. Tamoxifen is typically used for women that are pre-menopausal but also can also be used for women who are post-menopausal.
-
Aromatase Inhibitors (AI) - oral medications that stop estrogen production in the adrenal glands. Aromatase inhibitors are typically used for women that are post-menopausal, but also can be used for women who are pre-menopausal and are taking an ovarian suppression medication.
- Three types of AI's include:
- Arimidex (anastrozole)
- Aromasin (exemestane)
- Femara (letrozole)
There are medications that can block the anti-cancer effectiveness of hormone-blockers so talk to your medical oncologist about what medications to avoid while on treatment.
Side Effects of Hormone Blockers
Not everyone experiences side effects of hormone blockers, but like any medication, they have the potential risk of side effects.
Knowing that the hormone-blockers can reduce the risk of the breast cancer coming back often helps women stay with the medication despite the side effects.
Some of the potential side-effects of Tamoxifen:
-
Menopausal Symptoms
- Hot flashes
- Vaginal dryness or discharge
- Abnormal vaginal bleeding or loss of menstrual cycles
- Loss of libido
- Frequent UTI's
-
GI Symptoms
- Nausea
- Constipation
- Weight gain
- Leg swelling
- Mood swings
- Depressing
- Headaches
- Brain fogginess
- Fatique
- Weakness
- Bone pain
- Dry skin
- Hair loss
-
Beneficial side effects
- Helps stop bone loss after menopause
- Lower cholesterol levels
In rare instances, Tamoxifen can cause uterine cancer, blood clots and stroke.
Some of the potential side-effects of aromatase inhibitors:
- Bone, joint or muscle achiness/bone thinning/broken bones
- Brain fogginess/mood disturbances
- Insomnia
- Heart problems/peripheral edema/high blood pressure
- Hot flashes
- Stomach upset/nausea/vomiting
- Decreased energy
- Headache
- Elevate cholesterol levels
Not all side effects are listed above. It is recommended that you carefully review the package insert to educate yourself and inform your healthcare provider if you experience any unusual symptoms.
In some circumstances, women may go through a “menopause transition” while on Tamoxifen and become post-menopausal. These women may switch to an AI after 2-3 years.
While studies have shown that Tamoxifen is associated with preservation of bone mineral density, AI’s can have the opposite effect, often contributing to net bone loss.
Therefore, the following is recommended while on an AI:
- Baseline bone density test and repeated every 2 years
- Exercise regularly to increase bone strength
-
Adequate amount of calcium in your diet
- Dairy products, almonds, broccoli, kale, salmon, sardines, tofu
-
Adequate amount of Vit D in your diet
- Fortified dairy products/tuna/egg yolks/liver
- No smoking
- Limit drinking alcohol
-
Calcium and Vit D supplements (pharmaceutical grade or USP)
- Discuss the recommended dose with your physician
Targeted Therapy
Targeted therapies are a class of anti-cancer medications that are used to treat HER2+ breast cancers. Through research, drug development and clinical trials, we have been able to learn more about the changes in cells that cause cancer and the drugs that target them. These newer drugs are not a type of chemotherapy but are a “targeted therapy” that specifically targets those changes in cells.
Your medical oncologist will weigh many factors to determine if you will need targeted therapy or not:
- Stage of te disease
- Prognostic status (estrogen/progesterone/HER2)
- Size and location of the tumor
- Patient general health status
Targeted therapy is given through an intravenous line the same way chemotherapy is given, and it treats the body systemically, killing cancer cells throughout the body. It is typically used in combination with chemotherapy or another targeted therapy and can be continued after chemotherapy is completed*.
There are a variety of targeted therapies that are available to treat breast cancer today. The type of medication(s) and duration of treatment will vary based on your unique situation. Your medical oncologist will determine what treatment(s) is best for you.
For women with a metastatic hormone receptor-positive (estrogen-receptor positive and/or progesterone receptor positive) breast cancer, certain targeted therapy drugs are given in pill form and can be very beneficial to help stop or slow cancer growth.
These medications are typically given in combination with hormone therapy.
*For more information on targeted therapy, talk to your healthcare team or visit www.chemocare.com.
Side Effects of Targeted Therapy
Your medical oncologist will discuss the possible side-effects of targeted therapy*
These side-effects are typically mild, but there are some rare side-effects your physician will review with you:
- Diarrhea
- Heart damage which can lead to congestive heart failure (rare)
- Shortness of breath
- Leg swelling
- Severe fatique
- Hand-foot syndrome (hands and feet become red and sore)
*Targeted therapies are not indicated for women who are pregnant. If you are of child bearing age, talk to your medical oncologist about using effective birth control if you are prescribed these medications. Not all side effects are listed above. For more information on the possible side effects of targeted therapy, visit www.chemocare.com.
Immunotherapy
The most common type of side-effects of immunotherapy are:
- Skin reactions (dryness or cracking, blistering, redness, inflammation around the nails)
-
Flu-like symptoms:
- Fatique
- Body aches
- Fever/chills
- Weakness
- Nausea/vomiting
-
Other less common side effects include:
- Shortness of breath
- Diarrhea
- Fluid retention (edema)
- Cough/sinus congestion
- Headaches
*Not all side ef ects are listed above. Talk to your healthcare team if you experience side effects from your immunotherapy. Do not wait until symptoms become severe. In many cases, medications to suppress your immune system can be given to help reduce the side effects. For more information on possible side ef ects of immunotherapy, visit www.chemocare.com.
Some women have a family history of breast, ovarian, colon or pancreatic cancer and may be at a higher risk of developing a second cancer (in the same or opposite breast) or another type of cancer during their lifetime due to gene mutations in their DNA.
Your physician will review your heredity cancer risk at the time of your consultation and determine if you meet the guidelines for genetic testing.
There are a variety of sophisticated genetic tests available today that are performed by obtaining a sample of your blood or saliva. The test contains a panel of genes with each gene carrying a different risk for future cancers.
According to the American Cancer Society, the most common type of hereditary breast cancer is found in the BRCA1 or BRCA2 gene. Women with one of these mutations is not only more likely to develop breast cancer in her lifetime, but also at a younger age as well as to have cancer in both breasts. She is also at a higher risk to develop ovarian and other cancers in her lifetime.
If an inherited gene is found, treatment options can become more complex and the patient should consult with their healthcare team about the current guidelines of care.
Keep in mind that not everyone who carries a gene mutation develops breast or ovarian cancer.
Many patients with metastatic breast cancer gain great benefit from participating in a clinical trial study. During these studies, patients are able to receive novel (new) therapies to treat their cancer before they become FDA approved.
Clinical trials study new drug treatments and differ from normal care. These trials are usually sponsored by large organizations, such as drug companies, to collect and analyze data that lead to new treatments for metastatic breast cancer patients. This opportunity can offer real hope for metastatic breast cancer patients.
The benefit of participating in a drug study is that you will be a part of the research process and get access to tomorrow’s treatment today. Should you be interested in taking part in a clinical trial, you must meet the eligibility requirements of the study and sign a consent form prior to participation.

At the START Center, our mission is to provide the highest quality care for people with cancer and help accelerate the development of new treatments in order to improve patients’ quality of life and give them real hope against cancer.
In pursuit of this mission, the START Center provides world-class care, with multiple convenient locations in San Antonio and across the globe.
Comprised of a large team of caring, dedicated cancer doctors, the START Center combines excellent people, state-of-the-art capabilities and the most advanced treatments available.
We bring together multiple cancer-care specialties and modalities — surgery, chemotherapy, radiation therapy, immunotherapy, integrative therapies, genetic testing of tumors — for thorough and efficient care. In addition, we make an uncommon commitment to advancing the standard of cancer care through our leadership role in cancer research.

According to the American Cancer Society, there is no way to prevent a recurrence of cancer, but there are things that you can do to decrease your chances of a recurrence:
- Get regular screenings
-
Stay active and maintain a healthy body mass index (BMI)
- Getting at least 5 hours of exercise/week can decrease recurrence ≥ 30%
-
Eat well-balanced meals
- Reduced red meat intake
- Increase daily fiber intake
- Avoid trans fats
- Limit or avoid simple sugars
-
Anti-inflammatory diet
- Fruits/vegetables
- Omega-3 fatty acids
- Whole grains
- Lean protein
- Consume fish several times weekly
- Consume at least five servings of fruits and vegetables daily
- Consume folate rich foods daily (legumes, leafy vegetables, asparagus, eggs, beets, citrus fruits, etc.)
- Limit or avoid alcohol
- Do not smoke

After cancer treatment is completed, your healthcare team will set-up a post-treatment follow-up or survivorship care plan with you. The goal of this plan is to provide patients with an individualized care plan that addresses follow-up visits as well as long-term side effects of cancer and its treatments.
Each team will have its own set of guidelines for follow-up care, so talk to them individually to set-up a plan for your post-treatment needs.
Some of the services that can be expected during your follow-up care include:
-
Physician Visits
- Each specialist has their own set of guidelines for follow-up care
- Emotional well-being check
-
Imaging studies
-
Varies based on the type of surgery and age of the patient
- Mammogram, ultrasound, MRI, bone density test
-
Varies based on the type of surgery and age of the patient
-
Managing side-effects
- Medication education
- Ways to reduce side effects
- Physical therapy (if applicable)
-
Lifestyle modification recommendations
- Eat a healthy diet and exercise regularly
- No smoking
- Limit or avoid alcohol
- Avoid environmental toxins
- Get enough sleep
- Manage stress and surround yourself with supportive people
Images:
https://tefalhead.wordpress.com/
https://seer.cancer.gov/statfacts/html/breast-subtypes.html
https://hlp.nucleushealth.com/lumpectomy-and-mastectomy-appearance-after-surgery/view-item?ItemID=10385
National Cancer Institute:
https://www.cancer.gov/
Surveillance Research Program (SRP):
https://seer.cancer.gov/statfacts/html/breast-subtypes.html
American Cancer Society:
https://www.cancer.org/
ChemoCare
http://www.chemocare.com/
The START Center for Cancer Care
https://www.thestartcenter.com/clinical-trials/