Breast cancer is when a group of cells begin to divide and grow uncontrollably in the breast. Uncontrolled cell growth is dangerous because it can form clumps of cells that spread to other parts of the body. Clumps of cancerous cells can harm the digestive system, lungs, or blood vessels, and can also create chemical imbalances throughout the body.
Currently, breast cancer is the second leading cause of death for women worldwide (with lung cancer being number one). Although more women today are being diagnosed with breast cancer than in recent years, more women are surviving breast cancer than ever before as well!
Recent studies show:
- 1 in 8 women will be diagnosed with breast cancer
- 3/4 of women with breast cancer will survive more than 10 years
- 2/3 of women with breast cancer will survive more than 20 years
Why is breast cancer such a common type of cancer?
One reason is that women have higher amounts of certain hormones, such as estrogen, that make breast cancer more likely. Also, studies show that current societal trends such as having fewer children, breastfeeding less, higher rates of obesity, and increased lifespan, all contribute to higher rates of breast cancer.
Why are breast cancer survival rates increasing?
State-of-the-art treatments such as those offered at South Texas Oncology and Hematology for Cancer Care are helping to beat cancer faster and more effectively. Visit the START Center services page for more information.
Additional Resources:
Only a doctor can officially diagnose breast cancer, but you can help detect cancer earlier by keeping an eye out for the following symptoms. Consult your doctor if you notice:
- Breast growth, change of shape, or change of thickness
- Pain in the breast
- Inverted nipples or retracted nipples
- Change of nipple skin texture, such as peeling, scaling, or dimpling
- Discharge of white/yellow fluids or blood from the nipples
- Unusual lumps in the breast that do not go away. Keep in mind that not all lumps are cancerous, and some lumps come and go over time. Breast-checking is no longer considered the most effective detection method, but regular checks might still help to detect cancer early on, and you should let your doctor know if you find a new lump. Breastcancer.org provides helpful instructions on how to conduct a self-check of the breasts.
Additional Resources:
Here are some of the leading treatments for breast cancer, all of which are available at South Texas Oncology and Hematology for Cancer Care:
-
Genetic Testing
- Because every person is different, every cancer is different. Thus, your cancer treatment should also be personalized for you. And since your time is precious as a cancer patient, getting the most effective drug early on in your treatment process is critical. South Texas Oncology and Hematology for Cancer Care is the first cancer care provider in South Texas to offer genetic testing of tumors to help you get the best medication for your cancer as fast as possible.
What is genetic testing?
Genetic testing can help you determine your risk for cancer based on your genes. It can also help your doctor know the best medication for you. Each of your cells, including your cancerous cells, contains a copy of your DNA. By sequencing the DNA in your tumor, the cancer specialists at START can use a series of tests to identify which anti-cancer drugs are most likely to help fight your cancer. This can save you weeks to months of treatment and unnecessary side effects!
-
Anti-Cancer Drugs
- Most breast cancer treatments involve taking medication. START Center for Cancer Care provides comprehensive on-site pharmacy services including medication pick-up, counseling, financial aid, prior authorization processing for insurance claims, and even home delivery.
START Center Oncologists are leaders in international cancer research and conduct the world’s largest oncology program in Phase I clinical trials for anti-cancer medications. (Phase I trials are the first round of research trials for new medications. These types of trials use just a few participants.) The researchers at START have access to the very latest promising new anti-cancer medications.
Generally, a combination of different medications will be used together. Here are the most common types of drug treatments:
- Chemotherapy - Chemotherapy drugs will look for cells that divide quickly (like cancer cells) and destroy them. It is particularly useful when treating cancer in later stages because it can kill cancer cells throughout the whole body. More than half of cancer treatments involve some kind of chemotherapy, sometimes to completely remove the cancer and sometimes just to slow symptoms. You might have heard of chemotherapy side effects such as hair loss, nausea, or damage to the skin and or bones. These side effects occur because the tissue in your hair, intestines, skin, and bones are all fast-growing cells and thus might potentially be attacked by chemotherapy drugs.
- Targeted Therapy - Targeted therapies are better at attacking only cancer cells and leaving other cells alone. In some cases, targeted therapies do not cause as many side effects as other treatments because they are better at targeting cancer cells and leaving healthy cells alone.
- Immunotherapy - Immunotherapy drugs boost your immune system’s natural ability to fight your tumor. Tumors are good at avoiding the body’s immune system, so to improve your body’s response, immunotherapies include a variety of strategies such as adding extra T-cells and antibodies that specifically recognize and attack your tumor, introducing vaccines, or blocking the signals that would normally tell the immune system to slow down.
- Hormone Therapy - Research shows that abnormal hormone levels are the most significant cause of cancer. These hormones contribute especially to cancer in the breast: estrogen, progesterone, prolactin, and testosterone. Hormone therapies manipulate the balance of hormones in your body through oral intake, injections, or surgeries that remove hormone-producing organs.
-
Surgery - START surgeons have mastered any type of breast cancer surgery you might need. Different breast cancer surgeries include:
- Lumpectomy - Used for smaller tumors, lumpectomy removes just the tumor from your breast.
- Mastectomy - For more advanced stages of cancer, you might opt for a mastectomy, which is the removal of an entire breast. If you are at a high risk of developing breast cancer, you might even remove both breasts (a double mastectomy). Reconstructive surgeries are also available.
- Sentinel node biopsy - Lymph nodes are receptacles that help the body collect and filter out harmful cells, including cancer cells. Sometimes, cancer cells in your breasts concentrate in the lymph nodes (generally located in your underarms). A biopsy of your lymph nodes can indicate to your doctor that your body still contains cancer. In a sentinel node biopsy, a select few lymph nodes are removed to test whether cancer is still found in your breast.
- Axillary lymph node dissection - If cancer is found in the lymph nodes, a doctor might suggest an axillary lymph node dissection, which is the removal of several lymph nodes that contain cancer.
-
Radiation - Hitting cancer cells with high-energy particles can damage their DNA, which prevents the cancer from replicating and growing. Doctors will use different mechanisms to expose the cancer to radiation, and this treatment can take anywhere from three days to six weeks. South Texas Oncology and Hematology offers a variety of cancer-killing radiation techniques, such as:
- External beam radiation - External beam radiation targets a stream of high-energy particles at the tumor in your breast.
- Brachytherapy - Instead of shooting a stream of the radioactive particles at your body, brachytherapy involves inserting implants of radioactive materials directly into the body.
Additional Resources:
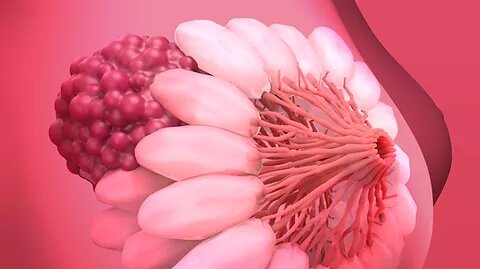
In many cases, breast cancer is caused by an improper balance of hormones. Hormones are chemicals produced by the body to trigger responses in other parts of the body. Breast cancer usually starts in the lining of breast ducts (the tubes that carry the milk to the nipple), which are controlled by hormones such as estrogen, progesterone, and prolactin. Most of the risk factors for breast cancer involve affecting your hormone levels in some way.
These risk factors include a mix of both genetic and lifestyle/environmental factors.
Genetic Factors
Generally, your genes can only increase your risk of getting breast cancer by 5-10%, although there are a few exceptions. Certain genes, particularly the BRAC1 and BRAC2 genes, drastically increase your risk of cancer. Studies show that a woman with the BRAC1 gene is 72% more likely to get breast cancer before the age of 80, and the BRAC2 gene increases the likelihood of developing cancer before the age of 80 by 69%.
Lifestyle/Environmental Factors
Here are several lifestyle and environmental factors that increase your risk of breast cancer:
- Consumption of alcohol - A recent study showed that drinking even one extra unit a day of alcohol increased the risk of breast cancer by 10% (a unit is half a glass of wine). Alcohol consumption increases breast cancer risk because it boosts estrogen levels.
- Obesity - Being obese after menopause accounts for a 7% increase in the likelihood of developing breast cancer. Fat cells are more likely to produce high levels of hormones.
- Number of children - A woman’s chance of developing breast cancer decreases by 7% with every child she bears. Many researchers believe that the increased incidence of breast cancer in westernized countries (which, by the way, is NOT seen in developing countries) could be halved if women in westernized countries had as many children as those in developing countries.
- Length of breastfeeding - Chances of getting breast cancer decrease by 4.5% for every 12 months spent breastfeeding. Some experts believe this is because the movement of fluid through the milk ducts keeps cancerous clumps from accumulating.
- Increased age - Cancer risk increases with age. As a woman lives longer, it is more probable that she will develop cancer.
- Hormone replacement therapy - Women who take additional hormones such as estrogen and progesterone have been found to have increased cancer risk.
Additional Resources:
Not all cases of breast cancer can be prevented, but there are several lifestyle changes you can make that will decrease your likelihood of getting breast cancer.
- Limit alcohol intake.
- Maintain a healthy weight – Weight can often be maintained through a healthy diet and exercise.
- Exercise – Studies show that exercise helps reduce the risk of breast cancer, possibly because it helps to maintain a healthy weight and possibly because it affects hormone levels in the body.
- Have more children
- Breastfeed for longer
- Take hormone supplements carefully – If you are concerned about your breast cancer risk, let you doctor know before using hormone replacement therapies.
- “Breast Anatomy.” Cleveland Clinic, the end of each, between the lobes and ducts.
- Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet. 2002 Jul 20;360(9328):187-95.
- Engin A. Obesity-associated Breast Cancer: Analysis of risk factors. Adv Exp Med Biol. 2017;960:571-606.
- Krusinska B, et al. Associations of Dietary Patterns and Metabolic-Hormone Profiles with Breast Cancer Risk: A Case-Control Study. Nutrients. 2018; 10(12)
- Kuhl H. Breast cancer risk in the WHI study: the problem of obesity. Maturitas. 2005 May 16;51(1):83-97.
- Scowcroft, Henry. “Why Are Breast Cancer Rates Increasing?” Cancer Research UK - Science Blog, 2 Feb. 2011, Source
- Tworoger SS, et al. Inclusion of endogenous hormone levels in risk prediction models of postmenopausal breast cancer. J Clin Oncol. 2014;32(28):3111–7
- Travis RC & Key TJ. estrogen exposure and breast cancer risk. Breast cancer research : BCR. 2013. 5(5), 239–247.