Inflammatory breast cancer (IBC) is a rare type of breast cancer that is different from non-inflammatory breast cancer in its symptoms treatment, and outlook. The skin of the breast can look red, swollen, thickened, or have an orange-peel appearance. The skin changes are caused by cancer cells blocking the lymph vessels in the skin causing the breast to look inflamed.
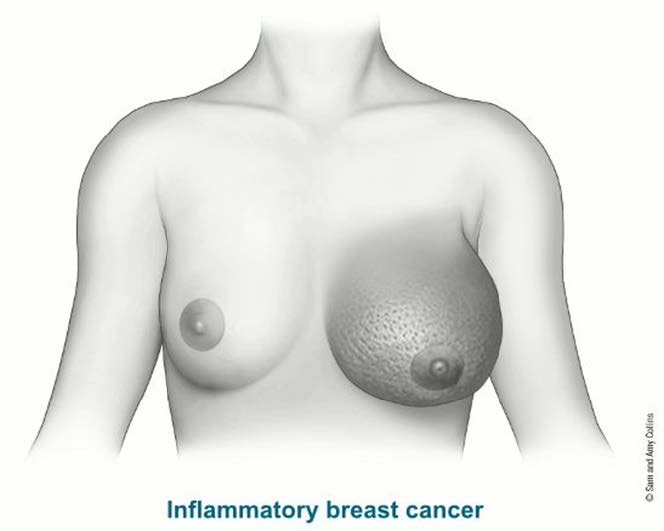
IBC tends to be more aggressive than most common types of breast cancer. All IBS starts at stage 3 breast cancer since it involves the skin of the breast. One in three patients with IBC will have distant metastatic disease. If metastatic disease is found, then it is classified as stage 4 breast cancer.
It is uncertain what causes breast cancer, but many studies point to a combination of factors, such as age, genetic predisposition, family history, reproductive factors, lifestyle behaviors, and environment.
Breast Imaging
Breast imaging tests such as a mammogram, ultrasound, and breast MRI take pictures of the inner part of your breast(s) so that a radiologist, a doctor that specializes in reading images, can take a closer look at your body.
-
Mammography uses X-rays to create images of your breasts
-
Screening Mammograms are done when there are no symptoms
- Example: annual mammograms
- Diagnostic mammograms are done when there is an area of concern
- 3D digital imaging or breast tomosynthesis is an advanced form of imaging that offers high-quality images from various angles, resulting in more accurate results vs. 2D imaging
-
Screening Mammograms are done when there are no symptoms
-
Ultrasound uses sound waves to create images of the breast tissue
- This procedure is often used in combination with a mammogram to evaluate areas of concern
- The procedure is painless
-
Breast MRI provides the clearest and most detailed pictures of the breast
- The MRI creates a 3-D image of the breasts
- Helps with staging and pre-surgery planning
- The procedure uses an IV contrast which is injected intravenously into the arm before the test. This contrast lights up during the exam, giving the doctor a better look at the breasts and surrounding areas
- The American Cancer Society recommends that all women that have a >20% lifetime risk of breast cancer, have a breast MRI and mammogram every year
Breast Biopsy
When a suspicious mass or an area of concern is seen on a mammogram or ultrasound, your doctor will order a breast biopsy to have a sample of the tissue examined to check for the presence of cancer cells.
After the tissue from the breast biopsy is removed, it is sent to a lab where a pathologist, a doctor that specializes in analyzing body tissue, examines the cells under a microscope and determines a diagnosis. The pathologist will interpret the tissue samples and prepare a report to share with the healthcare team.
The pathology report will contain some of the following information about the diagnosis:
- Procedure performed (type of biopsy)
- Specimen location (breast, axilla, lymph node(s), etc.)
-
Histology type (where the cancer originated in the breast)
- Ductal
- Lobular
- Phyllodes
- Other - such as tubular or mucinous
-
Grade status:
- Low - Grade I – cells look most like normal breast cells and are usually slow growing
- Intermediate - Grade II – cells look less like normal breast cells and are faster growing
- High - Grade III – cells look the least like normal breast cells and are usually fast-growing
-
Receptors/biomarkers status:
-
Hormone receptors
-
About 70-80% of breast cancers are hormone sensitive and include:
- Estrogen receptors (ER) and/or
- Progesterone receptors (PR).
-
About 70-80% of breast cancers are hormone sensitive and include:
- Hormone receptor positive breast cancers respond to hormone or endocrine therapy
-
Hormone receptors
-
HER-2 status:
- About 10% of newly diagnosed breast cancer patients are HER-2+
- HER-2+ is an over-expression of a protein called human epidermal growth factor receptor 2
- HER-2+ breast cancers respond to targeted therapies
-
Proliferation rate:
- Ki-67 – a test that measures the percentage (from 0-100%) of cancer cells that are actively dividing. The higher the proliferation rate, the faster the cells are growing and dividing
After a breast cancer diagnosis is confirmed, you will meet with a team of physicians that specialize in diagnosing and treating breast cancer. These specialists will include the following:
- Medical Oncologist
- General Surgeon or Surgical Oncologist
- Radiation Oncologist
- Lymphedema Specialist
Treatment options can vary based on your unique situation and can include a combination of the following:
- Chemotherapy
- Surgery
- Radiation therapy
- Targeted therapy
- Immunotherapy
- Lymphedema therapy
- Hormone-blocker or endocrine therapy
- Clinical trials (for metastatic breast cancer patients)
They will take into consideration factors such as your age, overall health status, type of breast cancer, and the stage of your disease.
After receiving an IBC diagnosis, you can expect to see a medical oncologist. A medical oncologist has extensive knowledge in diagnosing and treating cancer and pays special attention to the pathology report(s) from your breast biopsy(s). The information in the pathology report helps the physician determine the best treatment option for you. What’s more, the medical oncologist will discuss the risk of your cancer coming back after you have completed treatment.
Once your treatment plan is established, the medical oncologist will recommend the medication(s) most beneficial to you. The medication prescribed is considered “systemic treatment,” because it affects the entire body, not just the breast.
The goal of systemic treatment is to kill cancer cells and reduce the risk of cancer coming back in the breast and in other parts of the body, such as the organs and bones.
Chemotherapy
Chemotherapy is an anti-cancer medication that is either infused intravenously or given orally (by mouth) to fight cancer. The medication affects you systemically, traveling throughout the body to kill cancer cells.
Chemotherapy is almost always indicated for IBC. Your physician will weigh many factors to establish the best treatment plan for you:
- Stage of the disease
- Prognostic status (estrogen/progesterone/HER-2)
- Size and location of the tumor
- Patient general health status
If your medical oncologist feels you are a candidate for chemotherapy, it is almost always given first, called neo-adjuvant chemotherapy.
- Neoadjuvant chemotherapy (NAC) - NAC is a treatment (between 3 and 6 months) that is given before surgery with the goal of shrinking the tumor(s) or “downstaging tumors” before being removed with surgery.
Targeted therapy is given to women whose cancer is HER-2+ and it is not chemotherapy.
Targeted therapy is given through an intravenous line the same way chemotherapy is given, and it treats the body systemically, killing cancer cells throughout the body. It is typically used in combination with chemotherapy or another targeted therapy and can be continued after chemotherapy is completed*.
There are a variety of targeted therapies that are available to treat breast cancer today. The type of medication(s) and duration of treatment will vary based on your unique situation. Your medical oncologist will determine what treatment(s) is best for you.
For women with a metastatic hormone receptor-positive (estrogen-receptor positive and/or progesterone receptor positive) breast cancer, certain targeted therapy drugs are given in pill form and can be very beneficial to help stop or slow cancer growth. These medications are typically given in combination with hormone therapy.
Immunotherapy is a type of targeted therapy that helps boost the immune system to fight cancer. Drugs such as Pembrolizumab (Keytruda) are often used in combination with chemotherapy to treat cancer that cannot be removed with surgery (unresectable), or triple negative breast cancer that has spread beyond the breast to other parts of the body.
Specific eligibility criteria must be met for immunotherapy and your medical oncologist will help determine which treatment options are best for you.
*Targeted therapies are not indicated for women who are pregnant. If you are of child bearing age, talk to your medical oncologist about using effective birth control if you are prescribed these medications.
Hormone-Blockers
Hormone-blockers, also known as endocrine therapy, is prescribed for hormone receptor positive tumors and is a type of “systemic treatment,” meaning it affects the entire body, not just the breast.
The goal of a hormone-blocker is to kill cancer cells and reduce the risk of recurrence:
- Cancer cells have receptors (proteins) which attach to estrogen and progesterone in the body. The hormones “feed” the cells, making them grow out of control and spread
- Hormone-blockers can either stop the hormones from attaching to the receptors or stop estrogen production
The medication comes in pill form and is often taken daily for five years. However, some patients may benefit from taking the medication for 10 years or more, depending on the circumstances.
A medical oncologist will help determine which medication and duration is best for you based on your medical history, stage of disease and menopausal status.
Hormone-blockers are typically prescribed after local treatment (surgery or radiation therapy) has been completed. In some circumstances, a physician may prescribe the medication sooner if the disease has spread to other organs.
Two types of hormone blockers are:
- Tamoxifen – oral medication that blocks estrogen from attaching to cancer cells. Tamoxifen is typically used for women that are pre-menopausal, but also can be used for women who are post-menopausal.
-
Aromatase Inhibitors (AI) - oral medications that stop estrogen production in the adrenal glands. Aromatase inhibitors are typically used for women that are post-menopausal, but also can be used for women who are pre-menopausal and are taking an ovarian suppression medication.
-
Three types of AI’s include:
- Arimidex (anastrozole)
- Aromasin (exemestane)
- Femara (letrozole)
-
Three types of AI’s include:
There are medications that can block the anti-cancer effectiveness of hormone blockers, so talk to your medical oncologist about what medication to avoid while on treatment.
Systemic Treatment
Modified Radical Mastectomy
If the cancer improves with chemotherapy, surgery is the next step. (Surgery is typically not done for stage IV breast cancers.) The standard operation is a modified radical mastectomy, where the entire affected breast and lymph nodes under the arm (axilla) are removed. This is also referred to as a total mastectomy and axillary lymphadenectomy.
In a total mastectomy, the breast is removed along with overlying breast skin, nipple, and areola, leaving a flat contour to the chest following surgery. The goal of a mastectomy is the complete removal of the breast, removal of the underlying tumor with negative margins. Following a mastectomy, a small amount of breast tissue will remain within the fatty tissue below the skin.
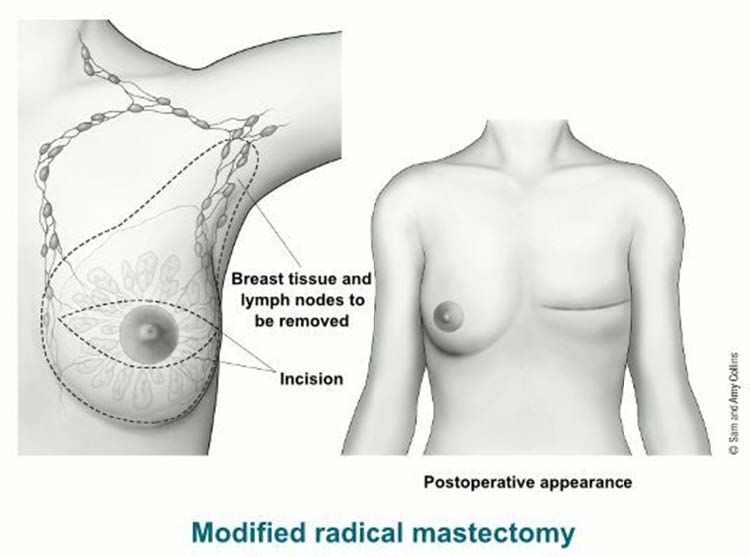
Because IBC affects both the breast and skin, breast-conserving surgery (lumpectomy) and skin-sparing mastectomy are not options. Axillary Lymphadenectomy.
The axillary lymph nodes, lymph nodes located in the underarm area, are among the first places that invasive breast cancer spreads. In an axillary lymphadenectomy, anywhere from 10-30 lymph nodes will be removed under the arm (axilla). This procedure is performed at the same time as the mastectomy. A possible complication of lymph node surgery is lymphedema (swelling of the arm). Speak to your surgeon about lymphedema prevention measures.
Most insurance companies will cover the cost of mastectomy bras, breast forms, camisoles, and prostheses. Ask your surgeon to write a prescription for these medically necessary supplies.
Breast Reconstruction Surgery
Breast reconstruction surgery is a treatment option for you to consider after a mastectomy. This procedure is done by a plastic surgeon, a physician who specializes in reconstructing the breast mound after a mastectomy. Due to the aggressive nature of IBC, breast reconstruction in this setting is typically reserved for the delayed setting (after completion of cancer therapies).
The goal of breast reconstruction surgery is to restore your breast(s) appearance and help you feel better about your body and the way you look in clothing after having a mastectomy. The plastic surgeon will talk to you about your treatment options, all the while, keeping in mind your lifestyle and personal preferences. Every woman’s situation is different and recovery times post-surgery can vary greatly based on the type of surgery chosen.
Radiation therapy is a local cancer treatment that uses high energy x-rays to kill cancer cells and shrink tumors. Radiation after mastectomy for IBC helps lower the risk of the cancer coming back in the treated breast or in nearby lymph nodes.
Radiation therapy is an outpatient procedure that typically starts after your surgical wound has healed (roughly 4 weeks). The radiation oncologist will set up a treatment plan specially designed for you through careful planning and mapping.
During this planning stage, you will be given special skin markings, which will aid in proper positioning for daily treatments. Radiation is given daily, Monday through Friday, for 6 weeks and each treatment takes only 10-15 minutes.

Radiation therapy can have short-term side effects from treatment which typically resolve within two weeks of completing treatment:
- Swelling
-
Skin changes to the treated area
- Sunburn appearance
- Redness
- Dry and flaky skin
- Darkening of the skin area being treated
- Fatigue
- Pain to the treated area
- Hair loss to the treated area
- Sore throat (if treated to the supraclavicular lymph nodes)
Many patients with metastatic breast cancer gain great benefit from participating in a clinical trial study. During these studies, patients are able to receive novel (new) therapies to treat their cancer before they become FDA approved.
Clinical trials study new drug treatments and differ from normal care. These trials are usually sponsored by large organizations, such as drug companies, to collect and analyze data that lead to new treatments for metastatic breast cancer patients. This opportunity can offer real hope for metastatic breast cancer patients.
The benefit of participating in a drug study is that you will be a part of the research process and get access to tomorrow’s treatment today. Should you be interested in taking part in a clinical trial, you must meet the eligibility requirements of the study and sign a consent form prior to participation.

Some women have a family history of breast, ovarian, colon, or pancreatic cancer and may be at a higher risk of developing a second cancer (in the same or opposite breast) or another type of cancer during their lifetime due to gene mutations in their DNA.
Your physician will review your heredity cancer risk at the time of your consultation and determine if you meet the guidelines for genetic testing.
There are a variety of sophisticated genetic tests available today that are performed by obtaining a sample of your blood or saliva. The test contains a panel of genes with each gene carrying a different risk for future cancers.

According to the American Cancer Society, the most common type of hereditary breast cancer is found in the BRCA1 or BRCA2 gene. Women with one of these mutations is not only more likely to develop breast cancer in her lifetime, but also at a younger age as well as to have cancer in both breasts. She is also at a higher risk to develop ovarian and other cancers in her lifetime.
If an inherited gene is found, treatment options can become more complex and the patient should consult with their healthcare team about the current guidelines of care.
Keep in mind that not everyone who carries a gene mutation develops breast or ovarian cancer.
At South Texas Oncology and Hematology for Cancer Care, our mission is to provide the highest-quality care for people with cancer and help accelerate the development of new treatments in order to improve patients’ quality of life and give them real hope against cancer.
In pursuit of this mission, South Texas Oncology and Hematology provides world-class care, with multiple convenient locations in San Antonio and across the globe.
Comprised of a large team of caring, dedicated cancer doctors, South Texas Oncology and Hematology combines excellent people, state-of-the-art capabilities and the most advanced treatments available.
We bring together multiple cancer-care specialties and modalities — surgery, chemotherapy, radiation therapy, immunotherapy, integrative therapies, genetic testing of tumors — for thorough and efficient care. In addition, we make an uncommon commitment to advancing the standard of cancer care through our leadership role in cancer research.

Images:
https://www.cancer.org/cancer/breast-cancer/treatment/surgery-for-breast-cancer/mastectomy.html
https://www.cancer.org/cancer/breast-cancer/about/types-of-breast-cancer/inflammatory-breast-cancer.html
National Cancer Institute:
https://www.cancer.gov/
Surveillance Research Program (SRP):
https://seer.cancer.gov/statfacts/html/breast-subtypes.html
American Cancer Society:
https://www.cancer.org/
ChemoCare:
http://www.chemocare.com/