Surgery is one of the common treatments you can expect after being diagnosed with breast cancer. When speaking with your surgeon, you will learn about the different surgical options that are recommended for you. These recommendations will be based on many factors:
- Stage of the cancer
- Lymph node involvement
- The size and location of your tumor
- The size of your breasts
- Your risk of cancer recurrence
- Personal preferences
Two of the main types of breast cancer surgeries are called partial mastectomy (or lumpectomy) and mastectomy, which are performed by a surgeon. If you choose to have a mastectomy, you will have the option to have reconstruction surgery, which is performed by a plastic surgeon.
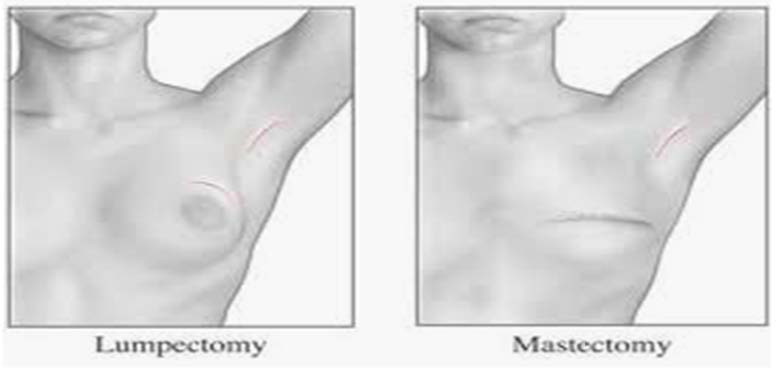
A partial mastectomy, also called lumpectomy, segmental mastectomy or quadrantectomy, is considered “breast-conserving-surgery”. During the partial mastectomy, the surgeon removes the tumor and a margin of surrounding healthy breast tissue. Axillary staging, biopsy of underarm lymph nodes, is required in most patients often using a technique called sentinel lymph node mapping.
The goal of a partial mastectomy is to remove the tumor with negative margins, determine if the tumor has spread to lymph nodes, and to preserve the appearance and shape of the breast.
A partial mastectomy usually does not require an overnight stay in the hospital and recovery time is typically less than a week. Your surgeon will give you post-op instructions, which we advise you follow closely.
**It is important to take into consideration that if you choose breast-conserving surgery, you will likely have whole breast radiation therapy as follow-up treatment.
A mastectomy is a surgical procedure involving the complete removal of the breast. Axillary staging, biopsy of underarm lymph nodes, is required in most patients often using a technique called sentinel lymph node mapping. The goal of a mastectomy is the complete removal of the breast, removal of the underlying tumor with negative margins, and to determine if the tumor has spread to lymph nodes. The amount of breast tissue left behind is influenced by the type of mastectomy performed.
Mastectomies can be categorized into several different types:
-
Nipple-sparing mastectomy –
- The breast tissue is removed preserving the overlying skin, nipple, and areola. This technique is utilized in patients pursuing breast reconstruction. Candidacy for nipple preservation is influenced by tumor location and prior breast surgeries.
-
Skin-sparing mastectomy –
- The breast is removed preserving the overlying skin but removing the nipple and areola. This technique is utilized in patients pursuing breast reconstruction.
-
Simple mastectomy -
- The breast is removed along with overlying breast skin, nipple, and areola. A simple mastectomy leaves a flat contour to the chest following surgery.
-
Modified radical mastectomy –
- The breast is removed, and an axillary lymph node dissection performed. See Types of Axillary Surgery.
If you choose to have both breasts removed, this is called a double mastectomy. If you choose to have your breasts removed when you do not have breast cancer but are at high-risk for getting breast cancer in your lifetime, this procedure is called a risk reducing or prophylactic mastectomy.
After a mastectomy, you can expect to stay in the hospital one or two nights, depending on your circumstances. You will go home with a special mastectomy bra or binder and small plastic drain(s) that comes from your surgical site(s) and collects fluid while you are healing. The drain(s) will be removed later during a post-op visit with your surgeon.
Recovery time will vary depending on the type of procedure(s) you had done. Women that choose immediate breast reconstruction during their mastectomy will have a longer recovery time vs. women that choose not to have breast reconstruction or delayed breast reconstruction. Your surgeon will give you post-op instructions, which we advise you follow closely. Typically, you can go back to regular duties after two to four weeks.
Whether you choose to have a partial mastectomy or a mastectomy, the recurrence rate remains about the same at approximately 10% in the treated breast and about 0.5% in the breast that has not had treatment.
The axillary lymph nodes, lymph nodes located in the underarm area, are often the first location of breast cancer spread. Consequently, surgical removal of one or more lymph nodes is often necessary in the staging and treatment of breast cancer.
- Sentinel lymph node mapping -radioactive dye is injected into the skin of the breast prior to surgery. This dye travels via the lymphatic vessels to the first lymph node(s) draining the breast, referred to as the sentinel lymph node. This lymph node is identified using a radioactive probe and removed at the time of surgery. The goal of sentinel lymph node mapping is to accurately stage the axilla while limiting the extent of axillary surgery, thereby minimizing the risk of lymphedema.
- Axillary lymph node dissection -surgical removal of lymph nodes within the underarm area. Axillary lymph node dissection is often required in patients whose cancer has spread to axillary lymph nodes, and if required the risk of lymphedema is increased.
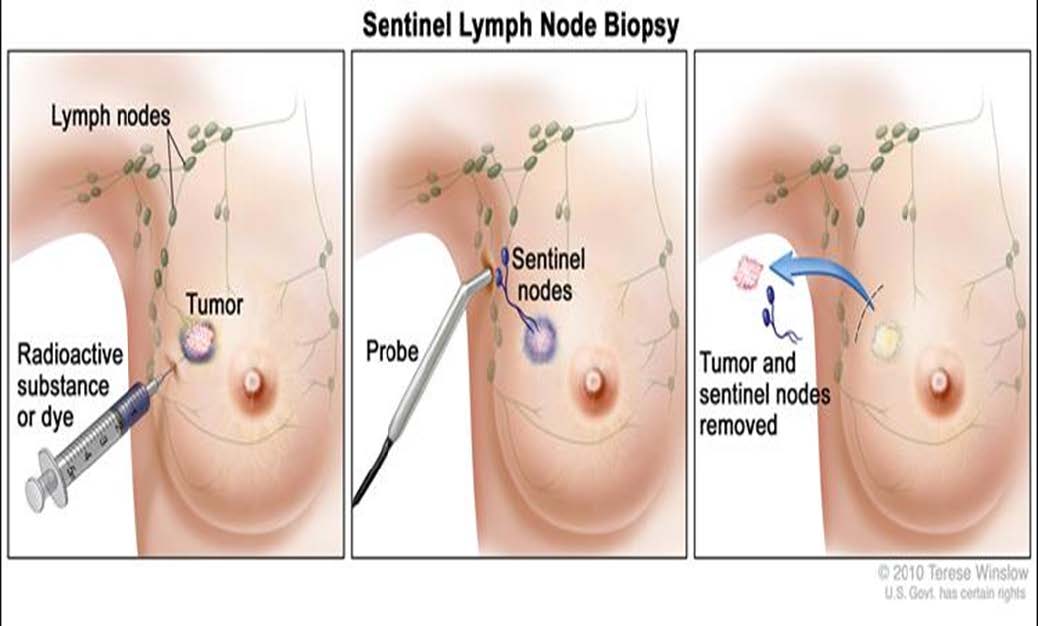
*In some instances of stage 0 breast cancer, a sentinel lymph node biopsy is not required. Talk to your surgeon to learn more about sentinel lymph node biopsies and what is recommended for you.
Breast reconstruction is a surgical treatment option if you choose to have a mastectomy. To learn more about breast reconstruction surgery, ask your surgeon to refer you to a plastic surgeon. They can provide you with information on how they can assist in rebuilding your breast mound(s).
The goal of breast reconstruction surgery is to restore your breast(s) appearance and help you feel better about your body and the way you look in clothing after having a mastectomy.
Keep in mind that every woman’s circumstance is different, and the plastic surgeon will discuss the breast reconstruction surgery options that are recommended for you.
These recommendations will be based on many factors:
- Stage of the cancer
- Lymph node involvement
- The size and location of your tumor
- The size of your breasts
- Your risk of cancer recurrence
- Personal preferences
In some cases, the breast reconstruction surgery can be done at the same time as the mastectomy, which is called immediate breast reconstruction.
In other cases, you may have to undergo additional treatment (such as radiation therapy) and breast reconstruction surgery is delayed until treatment is completed, which is called delayed reconstruction.
After breast reconstruction surgery, you can expect to stay in the hospital two nights or more, depending on your circumstances. You will go home with a special mastectomy bra and small plastic drain(s) that come from your surgical site(s) and collects fluid while you are healing. The drain(s) will be removed later during a post-op visit with your plastic surgeon.
Recovery time will vary depending on the type of procedure(s) you had done. Your surgeons will give you instructions on post-op care with restrictions that you should follow closely. Typically, you can go back to regular duties after four weeks.
** Insurance companies typically cover breast reconstruction surgeries, but we advise you check with your insurance company first to ensure you are well-informed about your coverage and options.
Types of Breast Reconstruction Surgeries
Implants and autologous reconstruction are two common types of breast reconstruction surgeries that are available to you in the San Antonio area. Your plastic surgeon will discuss the reconstruction surgery options that are recommended for you.
Implants
Implants are available in many different shapes and sizes and are made of silicone or saline. It will be up to you and your plastic surgeon to determine which size and type is best suited for you.
Breast reconstruction with implants is typically done in separate stages:
-
Stage One –
- A tissue expander is placed under the skin or under the breast muscle at the time of the mastectomy. This expander is slowly filled at the doctor’s office until the desired size is achieved, and the tissue has relaxed.
-
Stage Two –
- Once the expander has reached the desired size and the breast tissue has relaxed (about 3 months), the expander is exchanged with an implant.
- In some cases, the plastic surgeon does not have to prepare the breast tissue with an expander and is able to go directly to implant at the time of the mastectomy. Talk to your plastic surgeon to see if you are a candidate for this type of surgery.
-
Stage Three -
- In cases where your areola and nipple are removed during the mastectomy, you will have the option to have nipple reconstruction and/or tattooing after your treatment is completed.
Autologous Reconstruction
Autologous reconstruction is when a “flap” of tissue containing skin, fat, blood vessels, and sometimes muscle from a part of your body is used to rebuild your breast. These flaps can be a pedicled flap or a free flap.
- With a pedicled flap, the plastic surgeon uses skin, fat, the attached blood vessels and sometimes muscle from an area of your body and moves it through the body to the breast area. Since the blood supply to the tissue is left intact, the blood vessels do not need to be reconnected when it is moved to the breast area. A common area used for this procedure is the latissimus dorsi muscle (LD flap) from the upper back area.
- With free flaps, the plastic surgeon cuts the skin, fat, blood vessels and sometimes muscles from an area of your body and reconnects the flap blood vessels to the breast blood vessels. This procedure is a specialized type of microsurgery that not all plastic surgeons offer. The most common area used for this procedure is the abdomen.
Common Types of Autologous Reconstruction Surgeries Include:
- DIEP flap – The inferior epigastric perforator artery (DIEP) runs through the abdominal area. The plastic surgeon harvests a free flap of skin, blood vessels and fat from your lower abdomen area and reconnects it to the blood vessels and tissue of your breast. This procedure is a specialized type of microsurgery and is the most common type of flap reconstruction.
- LD flap – The latissimus dorsi (LD flap) comes from tissue in your upper back area. The pedicled flap of skin, blood vessels and muscle are moved through your body to your breast area to rebuild your breast.
- TRAM flap - The transverse rectus abdominis muscle (TRAM) comes from your lower abdomen area. The TRAM flap can be a pedicled or free flap and includes the skin, fat and blood vessels as well as the muscle.
- GAP flap – The gluteal artery perforator (GAP) comes from your upper buttock area. The GAP flap is a free flap that includes the skin, fat and blood vessels of your buttock.
- TUG flap – The transverse upper gracilis free flap (TUG) comes from tissue of your inner thigh. The pedicled flap includes skin, fat, blood vessels and muscle of your upper inner thigh
Women who have had previous abdominal surgery or who are very thin and don’t have enough abdominal fat may not be candidates for a DIEP flap. Speak to your plastic surgeon to see which procedure best suits you and your lifestyle.

